*** This post was updated on 5 April ***
This rolling wrap of reaction to the election-eve Federal Budget compiles reaction to developments affecting health and healthcare, with a focus on the social determinants of health and health equity.
Read Treasurer Josh Frydenberg’s Budget speech here.
The Health Budget Portfolio papers are here; the Department of Prime Minister and Cabinet papers are here; the Department of Social Services papers are here (including plans to expand the Cashless Debit Card); and a statement by Indigenous Affairs Minister Nigel Scullion is here.
In summary
Medical and health groups have welcomed very targeted measures for primary care in the 2019-20 Federal Budget but there’s big disappointment across the health and social sectors over its failure to address structural reform, the social determinants of health, prevention and to take effective climate action.
Noting this is the 25th Budget in a row to refuse to deliver a real increase in Newstart, the Australian Council of Social Service said the Budget is about cuts – “tax cuts for people who don’t need them, guaranteeing more cuts in future to essential services and our safety net for people who rely on them’’.
Despite a projected $7.1 billion surplus, the effective freeze on foreign aid continues and there is no much-needed commitment on social and affordable housing, or for homelessness – nor action on negative gearing or other property investment benefits – and job seekers are excluded from the energy rebate.
Disability, social service and health groups have welcomed the $500 million commitment for the Royal Commission into violence and abuse of people with a disability, though there is concern it will not be sufficient for the broad-reaching review that is needed, and there is also alarm about diversion of unspent NDIS funds.
The Federal Government has got the tick from medical, health and hospital groups for a range of measures including access to cheaper medicines, bringing forward by a year the lifting of the freeze on GP rebates, the fast-tracking of a Rural Generalist Pathway for trainee doctors, and ongoing commitment to mental health, particularly on youth suicide.
The Australian Medical Association is particularly happy, declaring the Budget has set up a “genuine election competition on health policy”.
But there’s deep disappointment from the Australian Healthcare and Hospitals Association that there has been no shift on private health insurance subsidies or other major structural reform, and a lack of any concrete action on preventive health, which “has been allowed to slip down the health budget priority list again despite its proven benefits in preventing big health bills later”.
The Public Health Association of Australia awarded the Budget “at best a D-minus” on prevention, saying that “two of our biggest killers were conspicuous by their absence in the Budget – obesity and alcohol”.
“Like inaction on climate change, the budget does little to prevent a future illness tsunami,” said PHAA CEO Terry Slevin.
The PHAA has however welcomed investments in child dental benefits, “sorely needed” mental health and suicide prevention commitments, and Medical Research Future Fund (MRFF) guarantees ($260M over 10 years) for preventive and public health research plus another $160M in Indigenous health research over 11 years.
1. 350,000 older job seekers still left in poverty
Statement by COTA Australia
The Federal Budget again leaves almost 350,000 job seekers older than 45 years out in the cold by failing to increased Newstart payments and excluding job seekers from the energy rebate, Australia’s leading seniors’ advocacy organisation, COTA Australia, said today.
COTA CEO Ian Yates called on the Government to increase the Newstart by $75 a week and make sure all Newstart recipients can access the Government’s Energy Supplement the same as people receiving the Aged Pension.
Mr Yates said there are 183,000 people older than 50 on Newstart who have been on Newstart for longer than 12 months. Research shows if you’re unemployed longer than 12 months after age 50, you might not ever return to the workforce, in a large part because of ageist attitudes of employers.
“There are more unemployed workers between 55 and 64 than any other group of Australians and they receive Newstart income support payments longer than any other group as well,” Mr Yates said.
“Older workers face chronic age discrimination in the our workforce, which means finding work after 50 far more difficult, particularly in industries where workforce needs have changed over the decades.
“$40 a day – or $15,000 a year – is just not enough to survive on while people are actively seeking to return to the workforce. If people don’t have enough to cover the basics, people will be dealing with financial stress rather than working to build a future.
COTA’s recent survey ‘State of the (Older) Nation’ showed that Australians who were unemployed and renting between the age of 50 and 64 were facing the greatest level of financial stress, with 1 in 4 identifying energy bills as overdue because difficulties paying on time.
“At the same time losing a job often after nearly a lifetime of work, does mean the loss of savings and assets that may otherwise provide some financial protection in retirement.
“The inadequacy of Newstart contributes to undermining Australia’s retirement system and setting older workers up for poverty in retirement. We need to review the assets test for Newstart for people over the age of 50, as well as the rate ”
Mr Yates said it was inexplicable that Newstart recipients are not eligible to receive the $75 one off Energy Supplement announced in tonight’s Budget.
“Surviving on Newstart and looking for work after a lifetime of employment is soul destroying enough. Being told you aren’t eligible for the same help with bills as others receiving income support is outrageous and must be remedied immediately,” Mr Yates said.
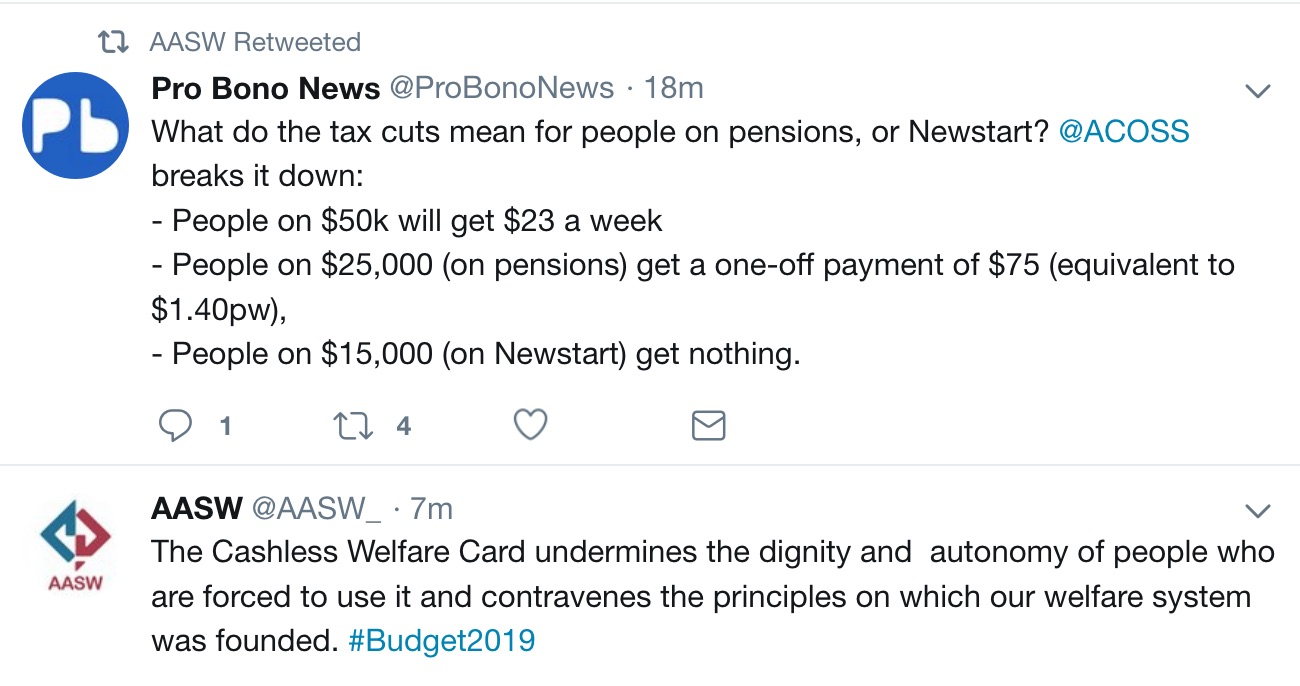
The Australian Association of Social Workers also raised concerns about lack of action on Newstart:

2. Record underspending on social housing in 2019 Budget as homelessness hits a record high
Statement by Everybody’s Home campaign
The Coalition Government has refused to acknowledge Australia’s growing housing crisis in the Budget announcement tonight.
Everybody’s Home, a national alliance of community, housing and homelessness organisations, called on the Treasurer for a fairer housing budget in a campaign leading up to today’s budget announcement.
“We called for urgent relief for the hundreds of thousands of Australians who are homeless, and more than 800,000 households going without basics to pay the rent,” Professor David Adamson, Everybody’s Home campaign spokesperson said.
“Last year, the Coalition had a chance to make a real move towards ending our housing crisis after shocking Census data revealed that homelessness in Australia had increased by 14% nationally and by 22% for people between 19 and 24. Unsurprisingly, they made no such move.
“For those seeking to rent a home on low income there are over 200,000 people waiting for social housing with a wait time often exceeding 10 years.
“So, while the Coalition announced a forecasted surplus of $7.1billion tonight, it means little to those 116,000 people experiencing homelessness or those 800,000 experiencing rental stress.
“The Federal Government continues to prop up the property sector with $11.8 billion in tax breaks but there’s nothing for ordinary Australians and renters who just want a home.
“It’s appalling that the Government knows that there will be 116,000 people experiencing homeless tonight and yet they have still chosen to favour property investors by continuing negative gearing and capital gains tax concessions.
“More than 800,000 Australian households have had to go without the essentials like food, just so that they can pay the rent. It’s not fair but it’s clear that fairness is not a priority for our current Government,” said Professor Adamson.
Everybody’s Home called on the Prime Minister, Hon. Scott Morrison, and Treasurer, Hon. Josh Frydenberg to rebalance the budget and:
Wind back the negative gearing and capital gains tax concessions to investors that cost billions in lost revenue.
Use these savings to kick start investment in the 500,000 social and affordable rental homes desperately needed by Australians on low and middle incomes.
Increase funding for homelessness services so we can end homelessness by 2030; and
Increase Commonwealth Rent Assistance by $20 a week to reflect the fact that rents have skyrocketed across the country.
“These were all practical, do-able solutions that would help make housing fairer and give every Australian the best chance to have a home,” said Professor Adamson.
3. Federal Budget sets up genuine election competition on health policy
Statement by AMA
AMA President, Dr Tony Bartone, said tonight that the Government’s Budget announcements have set up a genuine health policy competition for the upcoming election.
“The Health Minister, Greg Hunt, has listened closely to the AMA and delivered a strong Health Budget, with a particular emphasis on primary care, led by general practice,” Dr Bartone said.
“Australia’s hardworking GPs will be happy to see a commitment of almost $1 billion to general practice. This includes matching Labor’s promise to bring forward by a year the lifting of the freeze on rebates for a range of Medicare GP items.
“Overall, the Government has delivered a much-needed significant investment to general practice – the driving force of quality primary health care in Australia.”
The GP package includes:
- $448.5 million to improve continuity of care for patients over 70 with chronic conditions;
- Quality Incentive Payments for general practices ($201.5 million);
- $62.2 million for rural generalist training; and
- $187.2 million for lifting of the freeze on GP items.
The AMA also welcomes:
- Funding for new Pharmaceutical Benefits Schedule (PBS) medicines;
- Retention of the Aged Care Access Incentive (ACAI); and
- A rural workforce program.
Dr Bartone said there are obvious gaps in mental health, prevention, Indigenous health, pathology, and public hospital funding to improve allhospitals.
“We expect to hear more on these key areas from all parties before the election,” Dr Bartone said.
“Health Minister Hunt has worked closely with the AMA, especially on the primary care element of this Budget.
“Overall, the Government has produced a good start for a quality health policy platform for the election.
“We look forward to the Opposition making health a real contest when they roll out all their policies.”
Dr Bartone said there is still unfinished business with the Private Health Insurance reforms as they are implemented from this month, and with the ongoing work of the Medicare Benefits Schedule (MBS) Review, which must return any savings to new and improved MBS items.
The AMA Pre-Budget Submission 2019-20 is available at https://ama.com.au/sites/default/files/budget-submission/AMA_Budget_Submission_2019_20.pdf

4. Government turns its back on people who have the least, and guarantees more cuts to essential services
Statement by ACOSS
‘’The Government confirms its vision for our country is cuts, tax cuts for people who don’t need them, guaranteeing more cuts in future to essential services and our safety net for people who rely on them,’’ ACOSS CEO Dr Cassandra Goldie said tonight in response to the 2019 Budget.
The Government has announced a further $158 billion in tax cuts (plus an unknown cost from 2024 for cutting the 32.5% tax rate to 30%) on top of the $140 billion already legislated. Together this will deliver the largest tax cuts since the GST in 2000. The overall package gives the most dollars to people who already have the most, and offers people on the lowest incomes nothing:
People on $200,000 will get over $224 a week,
People on $50k will get $23 a week,
People on $25,000 (on pensions) get a one-off payment of $75 (equivalent to $1.40pw),
People on $15,000 (on Newstart) get nothing.
“None of the tax cuts benefit people on the lowest incomes, as one third of households, including low-paid workers, pensioners and people looking for paid work, do not have enough income to pay tax.
This Budget is the 25th in a row to refuse to deliver a real increase in Newstart.
In a mean-spirited move, people struggling on Newstart are even excluded from the token one-off cash payment of $75 to single pensioners ($125 for couples). The Government has once again turn its back on people who are going without food, unable to get their teeth fixed, trying to make ends meet on Newstart on $40 per day.
The unprecedented scale of these tax cuts also guarantees that many of the essential services people on low and middle incomes need will be cut in future, as they have been since 2014. People want to know that they can rely on schools, hospitals, child care, aged care and disability services and in the end that matters more to us than a sugar hit from tax cuts.
The budget does contain some welcome measures including $500 million for the Royal Commission into Abuse of People with Disability, an extra $80 million for young carers, $280 million for 10,000 home care packages for older people, $460 million for mental health, and the previously-announced $330 million in funding for domestic violence services.
These initiatives pale in comparison with the scale of need: the 3 million people in poverty, the crisis in housing affordability, the backlog of 100,000 aged care packages, the delays and under-spending on the NDIS, and the billions that need to be spent on mental and dental health.
It’s sad but telling that the Government has found just $5 million over 4 years to respond to the escalating crisis of suicide among young Aboriginal and Torres Strait Islander people.
“Far from dealing with these challenges, the Budget gets in the way by ripping another $158 billion from the public revenue base. We urge the Parliament to block any attempt to rush through the tax cuts in the final days before we go to an election, and instead commit to urgently increasing Newstart and Youth Allowance,” Dr Goldie said. 

VCOSS
‘Nada, zip, zilch, zero, diddly squat’…was the message from VCOSS CEO Emma King, who released the following statement:
That’s the level of real change last night’s federal budget delivered for the tens of thousands of Victorians on Newstart.
There were tax cuts for some and one-off pre-election cash payments thrown in for good measure.
But if you are among Australia’s most disadvantaged, struggling to find work and earn a decent wage, then this budget had nothing significant to help you.
What we need to do is increase Newstart to give people dignity and the support they need to build a better life.
This issue will now be front and center in the looming federal election campaign, and VCOSS will be in this fight.
We’ll be standing alongside our members, our national colleagues at ACOSS, economists and union leaders between now and polling day with a simple message for all those seeking office: it’s well past time to raise the rate.
5. Climate matters


6. Rural health responses
Few benefits for rural health in Federal Budget: statement by National Rural Health Alliance
The peak national body for rural health has welcomed $62m to train doctors in rural generalist practice, but says tonight’s budget has largely failed to address a critical shortage of allied health professionals for 7million people living outside metropolitan Australia.
National Rural Health Alliance CEO Mark Diamond said the budget was a mixed bag for rural health.
“We’ve had a big and much-needed focus on medical services and we welcome that but comprehensive health care needs paramedics, pharmacists, nurses and a whole range of other health professionals too. There was nothing in the budget to address this critical workforce shortage or to get them where they are so badly needed,” Mr Diamond said.
“And we were disappointed to see that major population health issues – obesity, maternity services, stillbirths or a national alcohol prevention strategy, all of which are well overdue for investment – were missing in the budget.”
Boosts for mental health including $15m for Indigenous suicide prevention, $114.5m for Adult Mental Health Centres, $263m for additional Headspace network sites and an $11.5m National Mental Health Workplace Initiative ($11.5m) sounded good but there was no indication these funds would be spent in the bush.
Some good news items for rural areas include $9.6m for alcohol and other drug treatment and support services, an expansion of the rural health outreach fund to increase access to pain management specialist services and train providers ($4.3m); a new Ambulatory Care Centre in Alice Springs ($25m); and other local service improvements including a new CT scanner for Bowen Hospital, an Early Psychosis Youth Centre in Darwin and new radiology, pediatric and chemotherapy services on the Bass Coast.
“We welcome an additional $160m for Indigenous medical research. It’s long overdue and we support it being targeted at rheumatic heart disease, and blindness and deafness in Aboriginal and Torres Strait Islander children and youth,” Mr Diamond said.
Last week’s National Rural Health Conference in Hobart called for governments to invest at least the same in addressing the allied and other health worker shortage as has been expended over many years in medicine.
“We still have regions in Australia where access to physiotherapy, dietetics, psychology, occupational therapy and podiatry services is severely restricted or even non-existent. How can that be?”
Rural doctors welcome further details on National Rural Generalist Pathway: Statement by the Rural Doctors Association of Australia (RDAA)
The RDAA has welcomed further details from the Federal Government on the implementation of the National Rural Generalist Pathway, following last week’s pre-Budget announcement of $62.2 million over four years to fast track the Pathway’s implementation.
RDAA has been a key driver over the past decade for the Pathway, which will deliver more of the next generation of doctors to rural and remote Australia with the skills to meet the needs of their communities.
“We are pleased that the additional details announced in the Budget are largely in line with key elements of the Pathway’s initial funding for which RDAA advocated strongly,” RDAA President, Dr Adam Coltzau, said.
They include:
Funding to support Australia’s two general practice colleges in obtaining recognition by the Australian Medical Council of Rural Generalist Medicine as a sub-specialty within general practice.
An expansion of the Junior Doctor Innovation Fund to provide additional rotations of medical interns and post-graduate Year 2 (PGY2) doctors into rural general practices and small rural hospitals.
The establishment of support and co-ordination teams to recruit, co-ordinate and support Rural Generalist training.
“The initial $62.2 million in funding for the National Rural Generalist Pathway is a significant win for RDAA, rural doctors and rural communities right around Australia” Dr Coltzau said.
“We again thank the Coalition for getting behind this important initiative, and the Australian Labor Party for committing to honour this funding should Labor be elected to government.
“This ensures that regardless of the outcome of the forthcoming election, this is one element of the Budget that we know will be delivered — and that is great news for rural and remote Australia.
“We also thank the National Rural Health Commissioner, Professor Paul Worley, and medical organisations that have worked with RDAA in making the Pathway a reality – including the Australian College of Rural and Remote Medicine, the Royal Australian College of General Practitioners, and the Australian Medical Association.
“RDAA has worked extremely hard over many years to establish the Pathway.
“We first advocated for the establishment of the National Rural Health Commissioner to drive the development of the Pathway. We then worked hard as a member of the Commissioner’s National Rural Generalist Pathway Taskforce and provided the lead on its Support, Incentives and Remuneration sub-committee.
“In addition to that work, RDAA developed and delivered a business case to the Federal Government and Department of Health on how best to implement the Pathway on a national scale.
“We are pleased to see that the core elements of our proposal have been included in the Pathway’s initial funding.
“The Pathway is a key part of the solution in addressing poor access to healthcare in rural and remote Australia. But it is not the only solution.
“The investment committed in the Budget provides a strong foundation, but there is more work and funding required to fully implement the Pathway, and there is more work to be done to ensure people living in rural and remote Australia have access to healthcare closer to home.
“Following the federal election, we’ll continue discussions with the elected government as to ongoing funding needs for the Program to ensure its full success.”
Rural Generalism boost in Budget welcomed by ACRRM
The Australian College of Rural and Remote Medicine (ACRRM) welcomes the commitment to funding for a National Rural Generalist Pathway as outlined in further detail in the Federal Budget announcement.
College President Dr Ewen McPhee says the four-year funding allocation of $62.2 million to support the application to the Australian Medical Council for recognition of Rural Generalist (RG) Medicine as a sub-specialty within general practice, the expansion of the Junior Doctor Innovation Fund, and establishment of support mechanisms for Rural Generalist training, provides the initial impetus for the ongoing development of the RG Pathway.
“As a long-time champion of rural generalism, ACRRM is committed to make a significant contribution to getting the National Rural Generalist Pathway up and running,” Dr McPhee says.
“We know this initiative will repopulate country towns with skilled Rural Generalists and improve health outcomes for rural and remote people by giving them greater access to the health care services much needed in their local communities.”
Dr McPhee also acknowledges the funding commitment to general practice.
“Lifting the freeze on MBS rebates for a number of MBS GP items will positively impact rural patients and rural practices,” he says.
“We also acknowledge the increased investment in the Practice Incentives Program and look forward to hearing more detail about the voluntary patient enrolment initiative for those aged over 70.
“These announcements, however, do not diminish the need for significantly more funding and structural reforms for General Practice to secure its capacity to deliver high quality, cradle-to-grave care into the future.”
Dr McPhee expresses hope that the Budget announcements, in particular funding for the National Rural Generalist Pathway, will provide a platform for further commitments to rural and remote health from all parties in the lead-up to the election.
“The College urges all political parties to address the ongoing disparity in health outcomes between rural Australians and their urban counterparts through proactive and targeted support in areas such as rural and remote mental health; Aboriginal and Torres Strait Islander health; and rural occupational health and safety,” he says.
7. Pacific Shuffle leaves behind children in need
Statement by World Vision
Australia’s largest humanitarian organisation World Vision has criticised the Federal Budget’s approach to aid, saying the government has shunned its responsibility to the world’s most vulnerable children.
Despite a $7.1bn budget surplus, the 2019-20 budget has plunged Australia further down the international aid rankings by continuing the freeze of an already depleted aid budget until 2022-23, when re-indexation will recommence.
World Vision Australia CEO Claire Rogers said the government has dressed up a new funding announcement in the Pacific as a boost to aid when it’s no more than a reallocation of funds from a cannibalised aid budget.
“This is not a Pacific step-up; it is a Pacific shuffle,” said Ms Rogers.
“The Government is shuffling money around the aid budget to make it look like it is bolstering development cooperation, but this could mean other communities are left behind.
“Australia’s increased involvement in the Pacific region should not come at the expense of
withdrawing from other parts of the world. It is unfair and strategically short-sighted.”
Ms Rogers is concerned funding for grants committed to the Government’s Australian Infrastructure Financing Facility for the Pacific operational from July 1, could be taken from aid supporting vulnerable communities in countries in South East Asia.
She said the government had failed to restore Australia’s reputation as a generous nation by not increasing its aid contribution this year.
“If the Government was serious about stepping up in the Pacific, it would show true leadership and invest additional funds in the region and grow the aid budget overall this year,” she said.
“Funding for infrastructure development shouldn’t come at the expense of current programs.
“Using existing aid funds for the new infrastructure investment bank would be robbing Peter to pay Paul. It would mean that life-saving development assistance to children and families in need in places like South East Asia could be diverted to fund Pacific infrastructure projects. The truth is that the Government can afford to do both.
“There is a need for the major parties to demonstrate real foreign policy leadership and make a bi-partisan commitment to increase aid by 10 per cent each year, to bring Australia’s contribution back into line with international standards.”
Any infrastructure projects funded by the new loan facility should reduce poverty, and be climate resilient, gender sensitive and compatible with other community development projects for the most impact, Ms Rogers said.
She added it was “extremely disappointing” that the government was still failing in this year’s budget to meet the commitment it made in the 2017 Foreign Policy White Paper to increase humanitarian assistance to $500m each year to address crises and conflicts. The $500m figure will not be met until next year’s budget, almost two years after it was first announced.
“Australia’s humanitarian aid makes a critical contribution to alleviating suffering around the world and needs to be scaled up now,” she said.
In a glimmer of good news, the government will end its freeze on indexation of the aid budget and tie it to CPI from 2022-23.
“News that indexation will be reinstated in four years’ time is welcome, but long overdue,” Ms Rogers said.

8. Mental health
Statement by the National Mental Health Commission
The NMHC is determined that tonight’s Federal Budget announcements will help fill the “real gaps” which have been identified in Australia’s approach to mental health prevention and intervention.
NMHC Chair, Lucy Brogden, said that suicide rates were still on the increase and suicide is now the leading cause of death among 15 to 34-year-olds.
“Just as tragic is the fact that Indigenous Australians are taking their own life at twice the rate of the non-Indigenous Australian population,” she said.
“Too many Australians are experiencing mental health conditions, issues which are more often than not preventable and treatable. The Commission will work to ensure that the right programs are put in place, along with the resources and dollars to match.”
Since 2012, the Commission has been working with the health and suicide prevention sectors, with lived experience, clinicians, academics and service providers to help build a system which supports all Australians across their lifespan.
“The Commission seeks ongoing consultation, to make sure that the impacts of programs and services are measured and that they are delivered to the people and places at most need,” Lucy Brogden added.
Some of the key take-outs from the 2018-19 Budget.
A real-time account of suicide underpins a renewed unified national focus.
An Australian Government-led national mental health workplace initiative will be priceless for the 12.6 million working Australians.
The Minister has also announced a revitalised plan for long-awaited dedicated support for mothers throughout their maternity journey and lastly, and the Government has invested in a trial of adult walk-in mental health centres in eight areas across the community.
As the lead agency in Australia’s largest collective commitment to mental health and wellbeing in our workplaces, the Commission will coordinate a four-year program for the Mentally Healthy Workplace Alliance with funds from this year’s Federal Budget.
The Commission looks forward to assisting the Government as it establishes a Special Adviser for Suicide Prevention within the Prime Minister’s portfolio. This position is expected to coordinate activities across the whole-of-government and assist in the design of essential services.
Lucy Brogden said these are all valuable initiatives but like all policies would require review and assessment.
“Access to quality mental health services and programs, regardless of your age, postcode or social and financial situation, is the foundation of our health system. Our mental health system needs to address barriers to access, and ensure that affordability are not barriers to wellness,” she added.
“We still have gaps in our current system, and inconsistencies in the delivery of connected support at all levels of need. The Commission is determined that these gaps and identified and rectified. We will continue to work closely with governments, private and community health providers, the mental health sector, carers and consumers, to ensure that everyone, regardless of where or when their need occurs, regardless in what setting they find themselves, has access to the support and care they need.
“This is a good start to build upon the great work and commitment that already exists in the mental health sector, and to build strong networks and resources for our workforce to address the critical needs for everyone who experience mental ill health in our workplaces.
“We are also acutely aware of the need to build up our mental health workforce so that they can deliver the services as and when they are needed. We need more people electing to study and work as mental health experts.
“The 2019 Federal Budget gives us hope but there is still much to do.”


Statement by Australians for Mental Health: Public funding for Adult Mental Health Centres welcomed but more investment needed
Grassroots mental health advocacy group Australians for Mental Health (AFMH) welcomes the Australian Government’s commitment of $114.5 million over five years for an adult mental health centre pilot program in Tuesday’s federal budget.
AFMH championed this proposal to publicly fund holistic and integrated after-hours mental health support for adults to fill a gap in the system. We congratulate Treasurer Josh Frydenberg and Prime Minister Scott Morrison on recognising its merit.
“Australians for Mental Health is extremely pleased the Government has rightly acknowledged that mental health is an issue of deep concern to all Australians and that suicide is a national tragedy,” AFMH Board Member and former Australian of the Year Professor Patrick McGorry said.
“This announcement of a pilot program for adult mental health centres is a landmark day for people with lived experienced, their families and the broader sector. The pilot is a good start and we look forward to seeing further investment,” Professor McGorry said.
“Mental health must be a bipartisan issue. The Shorten Labor Opposition must match and preferably surpass the Government’s mental health commitments, especially on adult mental health centres, in Thursday night’s budget reply speech,” Professor McGorry concluded.
This is a substantial achievement for Australians for Mental Health and reflects the importance of grassroots movements in Australian advocacy for health care.
AFMH looks forward to working with the Australian Government to carefully co-design this important pilot program before it is rolled out in 2020-21.
BACKGROUND ON ADULT MENTAL HEALTH CENTRES
The pilot program has received a total funding commitment in Federal Budget 2019-20 of $114.5 million over five years from 2020-21 to trial eight mental health centres that deliver a range of free, specialised mental health support services for adults requiring treatment, particularly after-hours.
As outlined in the budget, these centres will provide walk-in, coordinated care and advice for anyone with concerns, and will address what is seen by many as a missing gap in the health system. The centres will be rolled out in eight yet-to-be-determined locations nationally.
If implemented correctly this pilot program may serve as a model for a future larger investment of public funds in critical mental health services.
To be successful, these adult mental health centres must offer service navigation support, specialist psychiatric care, psychological services, social and community support services, drug and alcohol counselling, 24/7 assertive outreach and ambulatory care, consulting rooms for visiting specialists, facilities for GPs and allied health professionals, and online and telephone hotline services.
The funding commitment can be found at: – Budget Paper No. 1, Statement 1, Page 1-21; – Budget Paper No. 2, Part 2, Page 104.
9. Prevention and public health


Statement by Public Health Association of Australia: Not enough investment in disease prevention
The 2019 federal Budget does too little to prevent Australia’s major illnesses, according to Public Health Association of Australia CEO Terry Slevin.
“Australia is one of the lowest investors in illness prevention of any OECD nation at less than 2% of our national health spending,” Mr Slevin said.
“Two of our biggest killers were conspicuous by their absence in the Budget – obesity and alcohol.”
“Nonetheless this Budget has some valuable and welcome investments:
- Extension of the Child Dental Benefits Schedule ($1 Billion)
- Mental health and suicide prevention commitments ($736M) – these are sorely needed
- Research investment via the Medical Research Future Fund (MRFF) guarantees ($260M over 10 years) for preventive and public health research plus another $160M in Indigenous health research over 11 years
- Global health research focused on antimicrobial resistance ($28M) is welcome
- A tobacco control campaign at $20M over 4 years is a starting point, but smoking remains one of our biggest killers. We need to do much more to kick start serious tobacco control efforts.
- Promoting social inclusion and being physically active via sports ($23.6M)
- Take Home Naloxone Program ($7.2M)
“Spending on good health care, effective drugs and research is important and essential. But a continual downward spiral in real prevention is a trend we must seriously address.”
“We should have ambitious goals for real life-long health. To reach that point we need major action to contain the explosion of obesity and overweight in our community.”
“We need to do so much more to limit the harms of misuse of alcohol. And we have a massive gap to close regarding Aboriginal and Torres Strait Islander Australians.”
“But the long-term wellbeing of the community has not figured sufficiently in this budget,” said Mr Slevin.
“Like inaction on climate change, the budget does little to prevent a future illness tsunami.”
10. Health Budget 2019: cash splash beats long-term reform–again
Statement by Australian Healthcare and Hospitals Association
Commonwealth investment in healthcare is welcome—but a cash splash without long-term vision ensures that entrenched problems stay entrenched’, says Australian Healthcare and Hospitals Association (AHHA) Chief Executive Alison Verhoeven.
‘Tonight’s Budget once again rewards service volume and attendant rising costs when we need to shift the whole system to value-based healthcare—that is, better outcomes for patients relative to costs.
‘The Commonwealth Government has got some double bang for its buck as it re-announces previous promises as new Budget 2019 commitments.
‘Nevertheless AHHA welcomes access to cheaper medicines, specifically the re-announcement of new drugs to be added to the Pharmaceutical Benefits Scheme for breast cancer and skin cancer patients. Nearly $500 million for cancer research in Victoria is also welcome.
‘We note the Government has committed funds to a Royal Commission into violence and abuse of people with a disability—however this will not be sufficient for the broad-reaching review that is needed to ensure safe, high quality services for people with disability. We welcome funding for more home care packages, but this doesn’t go far enough to address the current long waiting lists in aged care.
‘AHHA supports the setting aside of $200 million to help reduce out-of-pocket costs for diagnostic imaging—but it remains to be seen how far this will go in reining in rising costs and in encouraging fee transparency.
‘It is pleasing that the Government has matched Labor’s promise to bring forward by a year the lifting of the freeze on GP rebates. Not addressing specialist rebates, however, will result in continuing growth in out-of-pocket costs.
‘Providing $62 million over four years to rural areas for GP, emergency care and specialist services is also welcome. But there is much more to do to in tackling issues of access and affordability for rural Australians—for example, funding a rural generalist program in allied health.
‘Another measure that does not go far enough is the re-announcement of $448 million over 4 years for payments to GP practices that ‘enrol’ elderly patients with chronic conditions. This expansion of the Health Care Homes trial provides a funding mechanism for team-based care, which should be made more broadly available.
‘It is disappointing that the Government has not funded a Productivity Commission inquiry into the private health insurance sector as part of reforming our public/private health system.
‘Private health insurers receive more than $6 billion of taxpayers’ money from the Government every year, and premiums continue to rise faster than inflation—often with reduced reimbursements for policy-holders. An independent review of this massive spend to ensure it represents good value for taxpayers is long overdue. The awareness program announced to support implementation of the gold, silver and bronze categories is not much more than window-dressing.
‘High on the agenda of most Australian households is the availability of affordable healthcare when we need it—and an expectation that our public hospitals will be therefore be well funded to provide these services. It’s disappointing the Commonwealth continues with its plan to claw back funding from the states for services already provided by our state-run public hospitals.
‘The lack of any concrete action on preventive health is concerning—it has been allowed to slip down the health budget priority list again despite its proven benefits in preventing big health bills later. Claiming previously committed funds for the Child Dental Benefit Schedule as an additional investment in prevention is a hoodwink.
‘Once again, dental health has been overlooked. It’s time to reverse the massive cuts to adult public dental services of the past few years. We also need to act now to fluoridate every community’s water supply in order to prevent costly dental procedures in the near future.
‘With a $40 billion investment over 4 years to improve access to medicines, it is very disappointing that the Government has not taken the opportunity to improve health outcomes for Aboriginal and Torres Strait Islander peoples by making the administrative changes needed to ensure patients discharged from hospital have access to Closing the Gap prescriptions. This is a practical and relatively inexpensive measure that would make a difference and has been overlooked for too long. Additional investment to support Indigenous health and medical research is welcome, however.
‘We applaud the ongoing commitment to investment in mental health, including to address youth suicide. The particular needs of young Aboriginal people must be part of this investment.
‘The lack of additional investment in harm minimisation and treatment services for alcohol and drug use is another disappointing gap in this year’s budget.
‘In summary we welcome the spending on health announced in tonight’s Budget. But we are disappointed that very little attention has been paid to the large structural reforms needed to deliver better healthcare access and affordability—piecemeal pot shots of cash do not make a budget’, Ms Verhoeven said.
‘AHHA and Australian health leaders have mapped out how to transform our healthcare system into a fit-for-purpose 21stcentury system. Healthy people, healthy systems (www.ahha.asn.au/Blueprint) is a comprehensive blueprint with a range of short, medium and long term recommendations on how to progressively reorientate our healthcare system to focus on patient outcomes and value rather than throughput and vested interests.
AHHA’s blueprint calls for an independent national health authority, distinct from the Commonwealth, and state and territory health departments, that would report directly to COAG, to tackle the entrenched problems facing our health services and to support better outcomes-focused, integrated care for all Australians.
11. Responses on disability-related policies
Royal Commission to bring justice for people with disability
Statement by People with Disability Australia
People with disability welcome the Federal Government’s commitment to fully funding our Royal Commission, as revealed in the 2019-20 Budget.
“We very much welcome the $527m allocated to our Royal Commission into the epidemic of violence, abuse, neglect and exploitation against people with disability, in tonight’s Budget,” said Matthew Bowden, Co-CEO of People with Disability Australia (PWDA), and member of Disabled People’s Organisations Australia (DPO Australia).
“We know that for people with disability to finally get the justice they deserve, the Royal Commission will need to come with a variety of essential supports and accessibility”.
“The Royal Commission must have this funding to make sure that different people with disability have their needs met, based on their personal circumstances, including age, sex, gender, sexual orientation, intersex status and ethnicity, acknowledging the particular situation of Aboriginal and Torres Strait Islander people and culturally and linguistically diverse people with disability.”
“The NDIS is an essential part of Australia’s social infrastructure, and must be available to all people with disability who need it. The almost $4 billion underspend of NDIS funds is a national disgrace, and we completely oppose the spending of these funds anywhere but on people with disability,” said Mr Bowden.
“People with disability come to us every day in despair because they can’t access the NDIS, their funding packages have been cut or they aren’t getting the supports they urgently need. Where is this money going, if it’s not being spent making sure that people with disability can have the supports they need for an equal life?”
“Staffing for the NDIS remains just over 3000, predicted to reach 3230 in 2019-20. As people wait for months to have their access requests and reviews assessed, the Government has failed to even meet its own target of 3700. The cap must be removed altogether so we are not left in limbo, sometimes at risk of harm and even death,” said Mr Bowden.
“We are disappointed yet again to see that the Federal Government has not listened to the 30% of people trying to survive on Newstart who have disability and/or illness, and lift them out of poverty. Newstart needs to be raised by $75 per week urgently.”
People with disability who cannot work deserve fair income support, but the Government has made the Disability Support Pension (DSP) harder and harder to access. That is reflected in this year’s Budget, where government spending on DSP is estimated to decrease by 2.3 per cent from 2019-20 to 2022-23. This is driven by the unfair tightening of eligibility, which simply drives more people into poverty on Newstart.
“In 2019, we want to make sure that all people with disability can have a safe, accessible and affordable home where we choose where we live and who we live with,” said Mr Bowden.
“We want to see any increases in NDIS pricing go to make sure that people with disability aren’t being forced to share their housing and supports. We know that institutionalised forms of housing, such as group homes, can increase the risk of violence and abuse for people with disability. People with disability need the same kinds of choice about where and who they live as non-disabled people have,” said Mr Bowden.
“Aboriginal and Torres Strait Islander people with disability were looking to this Federal Budget to outline how to address the multiple barriers to our participation within our own communities and the wider community,” said Damian Griffis, CEO of First Peoples Disability Network Australia, a member of DPO Australia.
“Our research shows that there is a higher rate of disability among Aboriginal and Torres Strait Islander people, and that those people experience higher rates of disadvantage. We wanted to see strong recognition of our expertise, and resources to address the barriers we face accessing the NDIS,” said Mr Griffis.
“Women are only 37% of NDIS participants, when we are the majority of people with disability. This is unfair, and shows that more investment is needed to get the NDIS working fairly for women with disability,” said Carolyn Frohmader, Executive Director, Women With Disabilities Australia, a member of DPO Australia.
“The employment statistics for women with disability have seen no improvement over the last two decades, showing how much we need targeted measures to provide a pathway out of poverty for women with disability. In addition, it is imperative that the Royal Commission fully investigate domestic violence against women with disability, who experience 37.8% higher rates than their non-disabled peers,” said Ms Frohmader.
“We want to end the discrimination that people with disability who come to Australia face. Many people with disability are routinely refused admission solely based on their disability,” said Dwayne Cranfield, CEO of National Ethnic Disability Alliance, a member of DPO Australia.
“Refugees, who come to Australia seeking protection and safety, have higher rates of disability than other Australians, and often can’t access the essential disability supports they need. We are disappointed to see further marginalisation of refugees in this Budget, through cuts to refugee employment services and asylum seeker support and no moves to address this glaring hole in our safety net. This will disproportionately target refugees and migrants with disability.”
“People with disability from migrant and refugee backgrounds have longer wait times to access essential supports such as the Disability Support or Aged Care Pension. This policy places them and their family at significant risk of financial hardship or poverty. We need to remove these barriers to social protection so culturally and linguistically diverse people with disability can access basic entitlements on an equal basis with other Australians,” said Mr Cranfield.
Funding win for disability Royal Commission – but advocates slam use of NDIS to bolster bottom line: Statement by the National Disability and Carers Alliance
Tonight’s announcement by Treasurer Frydenberg of more than $500 million being set aside for a Royal Commission into the violence, abuse, neglect and exploitation experienced by people with disability, has left disability advocates overjoyed.
“This Commission has been a long time coming,” said Chair of the National Disability and Carers Alliance (the organisation behind Every Australian Counts), Leah van Poppel.
“So many individuals and organisations have fought long and hard over many years to ensure the neglect, violence, exploitation and abuse of people with disability does not continue to be overlooked.
“The violence and abuse experienced by people with disability has been hidden in the shadows for too long. This Royal Commission will bring all these issues finally out into the light.
“$528 million over five years will ensure the Royal Commission has sufficient funding to be broad ranging and investigate the full range of abuse experienced by people with disability and the many places in which it occurs.
“This is a Royal Commission that must not only bring about decisive government and legal action – it must result in broader social change to ensure people with disability are able to live the lives they deserve, free from the fear of abuse, neglect or exploitation.
“Violence and abuse should always be above politics. This funding will allow the inquiry to be broad ranging, take the time it needs to fully investigate issues, and allow people with disability and their families to get the appropriate support to take part,” said Ms van Poppel.
However despite the Royal Commission win, disability advocates remain frustrated by the lack of attention given to the National Disability Insurance Scheme (NDIS).
While the budget figures are not clear on the current underspend on the NDIS, it does appears it now sits around $1.6 billion – contributing NDIS funds to be spend on the NDIS – not bolstering the budget bottom line to the overall budget surplus of $7.1 billion.
“NDIS funds must be spent on the NDIS – not bolstering the budget bottom line,” Ms Deane said.
“The NDIS has been underspent since its inception. This is a direct result of problems with the way the scheme is being implemented. People are waiting too long to enter the scheme – and once they do they are waiting too long for support.
“Most people in the NDIS are not spending all the funding allocated to them because they cannot work their way through the bureaucratic maze that is the NDIS to get the help they need. They are desperate for help and support – they just can’t get it.
“We have been holding forums across Australia and talking to thousands of NDIS participants, their families and carers. We know this $1.6 billion is urgently needed to fix the scheme and get it working the way it should so people aren’t left waiting for two years to get a wheelchair.
“This cannot be allowed to continue. Urgent changes must be made to get the scheme working the way it should and finally get people the help they need.
“Funds tagged for the NDIS should be spent on the NDIS. The underspend should be used to support people with disability and their families and fix up problems with the scheme – not returned to government coffers.
“Let’s be clear – we are not asking for more. We are simply asking for the finds allocated to the NDIS to be spent on the NDIS – not just quietly disappear. That’s what people with disability expect and deserve.
“The NDIS must run like a real insurance scheme – where money not spent is put away for a rainy day or invested back into the scheme to get it working the way it should.
“This money should be spent on the people who desperately need it most – people with disability, their families and carers,” said Ms Deane.
Federal Budget highlights the need for NDIS funding transparency: statement by National Disability Services
National Disability Services (NDS) has called for more transparency around the level of underspending in the delivery of the National Disability Insurance Scheme.
NDS Acting CEO, David Moody said “It’s disappointing the Government hasn’t been more transparent about the level of underspending for the NDIS this year. We are unable to confirm the exact amount.
“However, we note that the Government’s contribution to the scheme next year is $1.6 billion less than expected.
“The NDIS is a transformative social reform won through the united efforts of people with disability, their families and carers and providers across Australia.” Mr Moody said.
“That’s why our sector expects funds allocated to the NDIS to be invested in the scheme, and not be absorbed into general revenue for other government programs or to fund a surplus.”
In response to other budget announcements, NDS welcomed funding for the Royal Commission into the abuse of people with disability.
Mr Moody said, “The $527.9 million over five years should be sufficient to support the work of the Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability.”
About $379 million has been allocated to the conduct of the Royal Commission.
“NDS supports the remaining $149 million to assist people with disability to participate in the Commission,” he said.
12. Positive Bibs and bobs in Budget but too much ‘missing in action’
Statement by COTA Australia
Older Australians have some good news in today’s Budget but there’s very little real relief in the lead up to the Federal election, COTA Australia said today.
COTA acknowledges that the More Choices for a Longer Life package last year was a major commitment for older Australians and many of those measures are still being implemented this year, next year and beyond. However the momentum of More Choices has not been maintained with new initiatives in this Budget.
“We need a more integrated, robust and better resourced strategy to ensure government remains focused on the opportunities of Australia’s ageing population,” COTA CEO Ian Yates said.
“Yesterday’s report from the Parliamentary Budget Office’s signals greater action is needed today on policy initiatives for older Australians to mitigate the $36 billion cost to the Budget balance as a result of an ageing population and create positive opportunities.
“There are some good measures in this Budget but there are gaping holes – major initiatives missing in action – including
no extra Home Care Packages to reduce the nearly two year waiting list;
no increase in Newstart;
no oral and dental health program for older people; and
no proactive Retirement Incomes Review to future-proof our retirement income system.”
RETIREMENT INCOMES
The good news
The government’s announcement it will remove the work test for superannuation payments for Australians aged 65 and 66, recommended by COTA last year, is good news for those who can afford to make voluntary superannuation contributions, and will create a more flexible approach to retirement into the future.
What’s missing
A comprehensive retirement incomes policy.
“While we welcome the removal of the work test, this is another piecemeal measure among many inconsistencies, gaps and clunky components of the retirement income space and yet again demonstrates the need for a Comprehensive Retirement Incomes Review,” Mr Yates said.
“A Retirement Incomes Review would ensure government created equitable and fair policies across taxation, superannuation and the age pension and establish greater certainty for older Australians and people nearing retirement,” Mr Yates said.
HEALTH
The good news
$1.1 billion investment into Primary Health Care, in particular maintaining the current incentive for GPs to treat older Australians in residential aged care.
The re-introduction of indexation of GP Medicare payments and renewed focus on heart health in the form of Medicare funded heart checks.
$5 million investment in educating all Australians about the new private health insurance categories of Gold, Silver, Bronze and Basic.
“The Gold, Silver Bronze and Basic categories which commence this month will ensure that older Australians can compare their private health insurance more easily, choose the level of insurance that is most appropriate for them, and be confident that what they have chosen will be what is provided” Mr Yates said.
What’s missing
A comprehensive dental and oral health care scheme for pensioners and people living in residential aged care.
GP ordered MRI knee scans for Australians over 50.
“We’re deeply disappointed to still see the Australian Government actively discriminating on the basis of age in the provision of health care. While we support the $1 billion investment for children’s dental health, oral and dental health issues for pensioners and people living in residential care warrants priority attention,” Mr Yates said.
“There’s also absolutely no good reason why a 49-year-old can receive a knee MRI from their GP but once they turn 50 they’ll need to pay an expensive specialist to do the same thing.”
AGED CARE
The good news
$725 million of announcements in last Budget have been reaffirmed in this Budget, including 34,000 home care packages over the past 12 months (14,000 last Budget, 10,000 MYEFO 2018/19 and 10,000 February 2019).
$185 million investment in the Ageing, and Aged Care, and Dementia Mission of the Health and Medical Research Future Fund.
$7.1 million to address concerns about better use of unspent funds and align home care payment administration arrangements with other government programs.
$5.6 million investment on top of $7.7 million already announced funds to improve the compliance framework for the quality and safety of home care services.
$2.6 million towards the implementation of the Aged Care Workforce Strategy.
$1.5 million for serious incident response scheme requiring residential care providers to report a broader range of incidents occurring in the facility.
$84.3 million to expand the Integrated Carer Support Service.
“A $185 million investment into research into ageing and dementia will hopefully contribute towards improvements and discoveries that will this dreadful disease that is predicted to affect almost one million Australians by 2050,” Mr Yates said
What’s missing
Despite a $5.9 billion extension of the Commonwealth Home Support Program until 2021/22, the Government has continued to fail older Australians and aged care providers seeking future policy certainty on the foreshadowed single Care at Home Program.
The government has failed to invest any new funds into the Home Care Package waitlist since its department identified a $2.5 billion funding gap that is causing older Australian to wait more than 18 months for the care the government assesses them as needing.
“The counsel assisting the Royal Commission described the home care waitlist as ‘cruel, unfair, disrespectful and discriminatory against older Australians’ and we’d agree,” Mr Yates said.
“The government’s own department has told the Royal Commission it will only cost $2.0 billion to $2.5 billion a year to ensure older Australians wait no more than 3 months for the assessed level of care they need. The lack of investment in this Budget sends a troubling signal to the 125,000 older Australians still waiting for home care across the country.”
13. Enrolling for better health care
Statement by Consumers Health Forum
Older Australians will be able to enter an agreement with their GP to enable more personalised and coordinated care under a significant change announced in the Budget.
Under the new $448 million primary care scheme for patients over 70, general practices will receive additional payment for doctors and other clinicians to provide consultations, referrals, test results and scripts without having a face-to-face consultation with patients.
“This is a welcome development in bringing Medicare into the 21st Century by providing services and advice by doctors to patients without a face-to-face consultation as currently required under Medicare rules,” the CEO of the Consumers Health Forum, Leanne Wells, said.
“For many older people with chronic illness, getting to the doctor for routine checks and the like is a major challenge. More than half of Australians over 70 years have two or more chronic conditions.
“Older patients will also benefit from better follow-up and self-management support under these measures.
“These new arrangements will be voluntary for both patients and doctors and should encourage a more flexible and responsive approach to primary care, with the potential to reduce avoidable hospitalisation of patients. They will also help support older Australians to age in place.
“We would also liked to have seen the new scheme cover children five and under as part of this new approach to funding general practice care. Busy families also need access to flexible and affordable contemporary primary health care.
“We welcome the trial of a fresh approach to adult mental health with the development of eight walk-in centres to provide coordinated care and advice for people with concerns, to address what has been a gap in the health system.
“We are also pleased to see the Government will move ahead with plans to develop a new website to help consumers learn more about the out of pocket costs they might face for specialist medical care.
“The $7.2 million plan will include the publication of de-identified data showing the range of fees and out of pocket costs charged by specialists so that patients can identify typical specialist costs including when a course of treatment may involve more than once service, such as for breast cancer.
“A nationally searchable website for individual specialists’ fees will initially focus on cancer, gynaecology and obstetrics, areas where major concerns have been raised about costs.
“This Budget comprises a myriad of new funding measures for scores of different health initiatives in, pharmacy, medicines, hospitals, aged care and medical research.
“These initiatives are welcome but make more conspicuous the absence of a national strategic plan to combat one of Australia’s biggest health problems, obesity.
“Once again, a Federal Government has failed to devote any serious funding to a national population-wide public health scheme to encourage healthy diet and discourage promotion of unhealthy food to children.
“Yet as was demonstrated with a comprehensive anti-tobacco campaign, the benefits of a concerted public health campaign can be substantial,” Ms Wells said.
14. RACGP calls for more to be done in general practice
Statement by RACGP president Dr Harry Nespolon
General practice is Australia’s most accessed form of healthcare, with nearly 90% of all Australians visiting their GP each year. Despite this, funding for general practice represents only 7.4% of total government health expenditure including federal, state and local government expenditure.
Today’s announcements are a step in the right direction towards providing improved services to patients over 70. However, much more must be done to provide real access to primary healthcare to all Australians.
As President of the RACGP, I have been firmly advocating for a sustainable future for general practice.
These calls are starting to cut through the political noise and while the announcements today are not enough to secure a healthy future for general practice, they are a positive move in the right direction.
Practice Incentive Program – Quality Improvement
The $201.5 million over five years of additional funding to support practices administering the Practice Incentive Payment–Quality Improvement (PIP–QI) and the PIP Aged Care Access Incentive is a welcome investment, aimed at supporting quality improvement in general practice and the delivery of aged care services.
The RACGP is committed to improving the quality of care Australian patients receive whenever they visit their GP.
The RACGP is pleased to see that a number of concerns it raised regarding the proposed PIP–QI have been addressed, including the provision of additional funding.
The seven recommendations made, which have all been addressed, are;
- A profession-led Data Governance Committee to be established and funded by the Department of Health, to oversee the implementation of the PIP–QI
- The general practice profession to lead the development of Terms of Reference for the Data Governance Committee
- No general practice data collected in the first 12 months of QI–PIP is published
- There is re-confirmation that only the 10 quality improvement measures agreed to by Practice Incentive Program Advisory Group (PIPAG) will be required in order to access the PIP–QI
- The Primary Health Networks (PHNs) are provided with funding to upskill staff in data governance and practice support for quality improvement activities
- A formal review of PHNs, as PIP–QI data extractors and quality improvement providers, to be conducted within two years of operation, with a view to broadening eligibility for organisations providing these functions (e.g. medical colleges and the Australian Institute of Health and Welfare (AIHW)
- The RACGP and the profession to be provided with full access to any collected primary care data, including any additional improvement measures collected by the PHNs in addition to the 10 required for the purposes of PIP–QI
Addressing these concerns was central to RACGP supporting the program, as we believe the process had to address data privacy and quality. As the keepers of patient records, GPs want to make sure that any information is treated as our patients expect.
We believe these safeguards will ensure the integrity of patients’ data.
This funding will also pay for the continuation of the Aged Care Access Incentive, which was previously earmarked for removal, to support GPs going out to residential aged care facilities.
Patient enrolment
The RACGP commends the Australian Government on looking at new ways to better support our patients with the most complex needs.
The new patient enrolment system will initially be available for patients over the age of 70, who will be able to choose to register with a practice, which will be responsible for the management of their healthcare.
For every patient that enrols, the practice will receive a payment to support flexible care models. This may include a phone call following up with a specialist, email communications with the patient, telephone consultations, checking in with a family member or carer, or other related items that are essential for quality care but are unsupported by current MBS funding. This is additional funding, separate from MBS funding.
The announcement begins to acknowledge the full extent of what a general practice does when caring for a patient. For GPs, healthcare does not simply start and finish when a patient is with you in the practice. A continuous patient–GP relationship fosters a properly tailored and holistic health experience and has been proven to provide better health outcomes for patients.
The RACGP was pleased to hear from the Health Minister that this is the first stage of a universal telehealth service and hopes to see this program rolled out to the broader community sooner rather than later in order to ensure that no patient misses out on the benefits of well-delivered holistic general practice care.
Rural generalism
The RACGP welcomes the funding provided for the fast-track of a Rural Generalist Pathway for trainee doctors. This pathway will play a key role in ensuring Australians living in rural and regional communities have access to a highly trained GP who understands their individual needs and circumstances.
The specific training for rural generalist GPs will ensure that GPs and registrars have the right skills to practice in rural settings and can address the shifting needs of rural and remote communities, including the ever-evolving needs of mental health and palliative care.
$45m for primary healthcare research
The Federal Government has committed $45 million for primary healthcare research. The RACGP welcomes this long overdue investment.
Funding for general practice
The Federal government will provide $187.2 million over four years from 2019-20 to re-introduce indexation to all remaining general practitioner services on the MBS. While this is welcome, it won’t repair the damage caused by the Medicare rebate freeze over successive governments.
The RACGP will be advocating strongly for a significant investment in general practice in the coming Federal Election, because if something doesn’t change soon, I am fearful of patients’ ability to access care when they need, not when they can afford to.
Doctors Reform Society
In contrast, the Doctors Reform Society found little to celebrate, as their media statement makes clear:
“Last nights’ Federal budget seemed to forget that as doctors we see daily the challenges to access adequate timely high quality health care for many of our patients”, said Dr Tim Woodruff, President, Doctors Reform Society.
“No mention was made of ways to address the 8% of hospital admissions which could be prevented with better GP and community care (largely funded by the Federal Government). Forgotten also was the inadequate access to proper care in nursing homes because of lack of staff and access to GPs, leading to unnecessary admissions to under-resourced public hospitals. No mention was made of the years on elective surgery waiting lists for relatively simple procedures which might return a low paid worker to productive work but for the inadequate Federal funding of both primary community care and public hospitals.”
“Dental care wasn’t even mentioned despite the fact that dental procedures in public hospitals are the second most common reason for preventable hospital admission. All such patients need is adequate community dental care. It doesn’t happen. Waiting list for dental care extend to years and it doesn’t rate a mention. The Government has nothing to offer regarding the promotion of teeth rotting food and beverage. What will the Government do for our toothless patients?”
“The Government is to be commended for listing new expensive drugs for life threatening medical conditions but that’s been happening for years. It’s commitment to a specific suicide prevention strategy is great but isolated.”
“The boast is that there are less people on welfare. Welfare recipients struggle with health issues. We already have the most highly targeted welfare scheme in the OECD. It punishes deserving people and adds to their poor health. We see patients struggling with welfare issues far too often, with poor co-ordination with support services. Unemployable patients are given an unemployment benefit 40% below the poverty line. Whilst it’s great that people are encouraged to work if they can, many of our patients struggle. Robo-debt strategies make them sicker. The budget indicates further savings via supposedly even more efficient systems and if past performance is an indicator, even harsher treatment of welfare recipients”.
“It is disappointing that those with significant health care needs seem to be largely ignored or even further punished in this budget. Tax cuts can’t replace improved services.”
15. Psychologists welcome much needed mental health focus in Federal Budget
Statement by Australian Psychological Society
Australia’s peak psychology body has welcomed much needed investment in mental health programs to help ease the mental health crisis in Australia, as announced in the 2019 Federal Budget.
The Australian Psychological Society (APS) welcomes the Federal Government’s commitment of additional funding for mental health, including the setting up of walk-in adult mental health treatment centres, greater investment in youth programs through Headspace, healthy workplace programs, eating disorder centres and perinatal mental health support.
APS President Ros Knight said mental health issues in the community had reached crisis point in Australia.
“One in five Australians experience a mental health disorder every year, and mental illness is the third highest cause of burden of disease in Australia,” she said.
Ms Knight said the $114.5 million funding over five years for dedicated mental health treatment centres recognised the urgent need to better care for people experiencing mental health crisis however the investment could have been greater.
“Hospital emergency departments are not set up to care for people in severe psychological distress, particularly when drugs and alcohol are involved. These mental health centres are an important initiative and will provide people with access to healthcare professionals including psychologists trained to provide proper assessment and care.”
Ms Knight said psychologists were also encouraged to see $63 million in funding for six residential eating disorder treatment centres.
“It’s very difficult for people with severe eating disorders to access specialist residential care anywhere in Australia. Dedicated clinics will also enable healthcare teams including psychologists and dieticians to provide best practice care in a safe and appropriate environment.”
“This investment supports the Government’s proposed increased access to psychological services under Medicare for people with eating disorders,” said Ms Knight.
Ms Knight also welcomed $15.2 million funding for the Mentally Healthy Workplace initiatives to provide Australian businesses with strategies to achieve a healthy workplace.
Ms Knight said while the Budget has provided further initiatives for mental health there is still more that should be done.
“We believe a greater investment could be made in the prevention of mental health disorders and greater access to services for children under 12 years, and we would like to see further investment in capacity building in the rural mental health workforce and mental health research,” she said.
Ms Knight said: “We congratulate the Government on its strong investments in mental health and look forward to seeing further details and working with them to help deliver psychological care as part of a number of these programs.”
16. Research and science
*Correction issued by Australian Academy of Science and CSIRO*
CSIRO STATEMENT:
“The Australian Academy of Science’s statement that CSIRO has received a $21.5M funding reduction over the forward estimates is incorrect. The Government’s investment in CSIRO across this period remains consistent with previous levels, increasing by over $6m in line with indexation. This funding will continue to be directed towards innovative science and technology to solve Australia’s greatest challenges.”
AUSTRALIAN ACADEMY OF SCIENCE STATEMENT:
Based on the information available, the Australian Academy of Science’s media release in response to the Federal Budget stated that there had been cuts of $21.5 million over the forward estimates to the CSIRO. This analysis was derived by comparing the 2019/20 budget with the previous year’s budget over the forward estimates period.
Further information provided subsequently has clarified that the budget was referring to a reduction in the CSIRO’s total expenses, not a reduction in Government funding to CSIRO. The Academy understands that the Government’s investment in CSIRO across this period remains consistent with previous levels, increasing by over $6 million in line with indexation.
Mixed news for science in the 2019-20 Budget: Statement by Australian Academy of Science
The 2019-20 Federal Budget contains mixed news for science, with a number of very welcome announcements along with some damaging cuts to research programs.
Positive measures include $3.4 million new funding to support women in STEM, including the Science in Australia Gender Equity (SAGE) initiative led by the Australian Academy of Science and the Australian Academy of Technology and Engineering.
Also included are a raft of initiatives through the Medical Research Future Fund, $25 million new funding for coastal, environment and climate research, $56 million for nuclear medicine and waste management, $5 million for a dark matter particle research facility, $15 million for expanded outreach and education activities through Questacon, and $19.5 million over four years to establish a Space Infrastructure Fund.
Negatives include the abolition of the $3.9 billion Education Investment Fund which could have been used to support strategic research infrastructure; savings of almost $50 million from the entrepreneurship and industry research programs; and reductions in future allocations to university research, the CSIRO and Australia’s research grant programs totalling $389 million over four years.
President of the Academy of Science, Professor John Shine AC, said that while the Academy applauded the range of new initiatives, it was hoped that there would be more focus on science and innovation in the budget given the Government’s emphasis on knowledge and skills.
“It is counterintuitive to seek to produce a surplus by cutting the knowledge economy and by cutting funding to Australia’s key science and research agencies such as the CSIRO and the Australian Research Council,” Professor Shine said.
“The reductions in indexation of science and research programs over the forward estimates, resulting in cuts of $345 million to university research funding through the research support program are particularly concerning.”
“This budget also outlines cuts of $6.73 million to ARC research funding, immediately reversing part of the long-delayed return to indexation announced in the 2018-19 Budget, and cuts of $16.54 million to the National Collaborative Research Infrastructure Scheme (NCRIS) and $21.5 million over the forward estimates to the CSIRO.”
“Given the Government’s focus on economic growth it is disappointing that some of the very welcome announcements in this budget went hand in hand with these damaging cuts to Australia’s research programs” Professor Shine said.
FURTHER INFORMATION ON 2019-20 SCIENCE BUDGET MEASURES
Major science initiatives announced or elaborated in the Budget include:
$56.4 million over three years to the Australian Nuclear Science and Technology Organisation to support nuclear medicine production, critical radioactive waste management and nuclear decommissioning activities, and asset management. The Government will also provide an equity injection of $56 million to ensure the continued protection of both the community and the environment.
$25 million over four years for a coasts, environment and climate science research and education centre at Point Nepean, Victoria. The Centre will be led by Monash University and include an interdisciplinary research facility on marine and coastal ecosystems, climate science and environmental management.
$15.1 million over three years to expand Questacon’s education and outreach activities.
$3.4 million over four years to support women in STEM through the SAGE Initiative and a digital National Awareness Raising Initiative led by the Women in STEM Ambassador Professor Lisa Harvey Smith.
$19.5 million over four years to establish a Space Infrastructure Fund.
$5 million over two years to build the Stawell Underground Physics Laboratory to allow the University of Melbourne to join the global research effort to understand dark matter.
Funding of $2.9 million over three years to facilitate national leadership in agricultural innovation.
$3.6 million over two years from 2019-20 to trial a National Innovation Games through which students will work together to solve innovation, technology and/or digital challenges set by a corporate sponsor.
$0.5 million over five years (and $0.1 million ongoing from 2023-24) to establish an Australian Antarctic Science Council that would support reform initiatives announced as part of the Government’s response to the Australian Antarctic Science Program Governance Review 2017
Cuts and savings measures:
Abolishing the $3.9 billion Education Investment Fund and using the capital to establish a new Emergency Response Fund.
Savings of $48.9 million over five years from 2018-19 from the Entrepreneurs’ Programme and the Industry Growth Centres Initiative.
Reductions in indexation of science and research programs over the forward estimates resulting in cuts of:
$345 million to university research funding through the research support program. This is on top of numerous other cuts to university funding over the past several years.
$51,000 over the forward estimates to Australia’s four Learned Academies, including the Australian Academy of Science, the Council of Learned Academies and the Australian and New Zealand Association for the Advancement of Science.
$6.73M to ARC research funding, immediately reversing part of the long-delayed return to indexation announced in the 2018-19 Budget
$16.54M to the National Collaborative Research Infrastructure Scheme (NCRIS).
$21.5M over the forward estimates to the CSIRO.
***
AAMRI welcomes Government’s $20 billion commitment to medical research
The Federal Government has reaffirmed its commitment in the budget to building the Medical Research Future Fund (MRFF) to $20 billion by 2020-21. In addition, it has set a ten-year investment plan for the MRFF.
The President of the Association of Australian Medical Research Institutes (AAMRI), Professor Vlado Perkovic, said he was delighted the Government is sticking to its promises, and is pleased to see a new long-term vision for the fund.
“The ten-year investment plan is good news, it will allow our researchers to plan long-term projects that can deliver substantial health benefits to the nation,” said Professor Perkovic.
The Budget papers show that the fund is now at the half way mark, with the Government committed to it being fully funded within the next two years, making it the largest sovereign wealth fund for medical research in the world.
Professor Perkovic said that this new funding must now be spent wisely so that the maximum impact and value for money can be gained.
“As part of this long-term vision, it will be important to review how we are tracking over time. To make sure our investments continue to tackle the changing research priorities of the health system.”
Many of the existing funding opportunities from the MRFF have been administered through open competitive processes run by the National Health and Medical Research Council, something which Professor Perkovic said he was keen to see continue.
“The Government must now ensure that the vast majority of this new funding is awarded through rigorous competitive processes, so that we make the most of this opportunity and invest in the projects most likely to deliver,” said Professor Perkovic.
The new ten-year plan will see around $5 billion invested in medical research into some of the most chronic and debilitating diseases such as diabetes, cardiovascular disease, mental health, dementia and brain cancer.
It will also include investment in new clinical trials, allowing Australians world-first access to new drugs and treatments.
17. Beyond rhetoric, urgent need to reclaim fair-go society
Statement by Conny Lenneberg, Executive Director of the Brotherhood of St Laurence
A Budget is more than a fiscal document or set of policy priories. It is, as acknowledged by Treasurer Frydenberg, a test of values. As we steer into a federal election where the ‘fair go’ is taking centre stage in our political discourse, there are deeply jarring numbers that don’t figure in the Budget papers we must reckon with as a nation.
Here are two stark examples.
After 28 years of economy growth — a remarkable run of national prosperity — some 739,000 children under 15 live in poverty.
Newstart, a payment conceived to assist unemployed people while they hunt for work, has, perversely, become an impediment to gaining work. Today the daily rate is as little as $39.69 for a single person, effectively frozen for 25 years. There is strong community consensus that these barely subsistence rates are depriving our fellow Australians of their dignity let alone providing enough money to maintain housing and put food in the table.
Prime Minister Robert Menzies said the state owed its people “not only a chance in life but a self-respecting life”.
Prime Minister Ben Chifley, the architect of our post-war welfare system said: “The modern ideal is that there should be social security provisions to protect every citizen in his or her emergencies, from the cradle to the grave.”
Today, despite our progress, peace and prosperity, we fall short of the goals articulated by these two foundational Prime Ministers.
Bewildering to exclude people on Newstart from one-off energy payment
We need to urgently reclaim the fair-go society that we all cherish as Australians. The Brotherhood of St Laurence believes that means, as a priority, repairing our fraying social security system with its arbitrary compliance regime, invocations of so-called ‘welfare dependency’ and narrowing scope of who is ‘deserving’ — and who is not.
In this context, the decision to exclude Newstart and Youth Allowance recipients from one-off Budget payments to defray high energy costs is bewildering. A quarter of people on Newstart spend 10% of their income on energy and need such relief most of all in our community.
As we step into the federal election, the Brotherhood of St Laurence challenges all political parties to lay down a vision for Australia that is truly inclusive and takes full account of groups in our society that are excluded from our nation’s abundance: these include Aboriginal and Torres islander peoples, young people in our outer suburbs and regions struggling to get secure work, sole parents who are overwhelmingly single mothers and their children, mature aged workers displaced by structural shifts in our economy and older people contemplating their senior years without secure housing.
Our nation faces a pivotal economic and social moment with the challenge of climate change, record rates of underemployment alongside unemployment, the impact of technology and a housing affordability crisis that deeply impacts on people on very low incomes.
The risks are great for the resilience of our society, and especially for the most disadvantaged Australians. For the health of our economy and society, we need to invest in building people’s skills and abilities so they can participate in mainstream Australian life.
Most of all, we need the right policy settings for the emerging generation – this means thoughtful investment in supports for our children, young people and their families. Tax cuts are not the policy prescription we need at this critical time.
Meeting our long-term intergenerational challenges is a task framed by several budgets: requiring ongoing investment in our social infrastructure and systems, which are just as important as physical infrastructure of roads, rails, bridges, dams and ports.
Social policy must be integrated with economic policy so that, beyond rhetoric, we achieve the fair go we yearn for as fair-minded Australians.
18. Welcome funding for medical research and mental health – but more work needed to address Australia’s drug and alcohol service crisis
Statement by St Vincent’s Health Australia
St Vincent’s Health Australia – Australia’s largest not-for-profit health and aged care service provider – has welcomed the Morrison Government’s funding initiatives across the portfolio but says more must be done to support Australians struggling with alcohol and other drug problems.
“There’s much to welcome in the areas of health and aged care in this budget, but I’m concerned some of our most vulnerable citizens have been overlooked,” said Toby Hall, St Vincent’s Health Australia’s CEO.
“St Vincent’s is a partner in three of Australia’s leading medical research institutes – the Victor Chang Institute, the Garvan Institute and St Vincent’s Institute of Medical Research – so, of course, we’re happy to see the Government’s continued emphasis on medical research in this year’s budget.”
St Vincent’s Health will benefit from $30m in funding for the Aikenhead Centre for Medical Discovery, Australia’s first biomedical engineering research hub which will be built at St Vincent’s Hospital Melbourne.
“The Aikenhead Centre will be unique in Australia and rare in the world. It will be Australia’s first biomedical engineering research hub integrated with a hospital – and that’s what it makes it different to anything else happening in our country.
“By bringing scientists, engineers and students together with patients for the first time, Aikenhead will create collaborations to accelerate new discoveries in a way that is not currently available at any other clinical research campus in Australia. It will halve the time it takes to find breakthroughs and turn them into life-saving and life-changing treatments.
“As a provider of mental health services at our public hospitals in Melbourne and Sydney, we welcome the Government’s focus in this area and we’ll watch with interest the trial of eight specialist mental health hospitals to help people when and where they need it.
“The investment in Indigenous suicide prevention is also worth noting given the desperate need for support among young Aboriginal and Torres Strait Islanders.”
However, Mr Hall said he was disappointed at the budget’s lack of emphasis on one of Australia’s hidden crises: the half a million people who are unable to access alcohol and other drug treatment services.
“Last week, St Vincent’s along with 20 other organisations called on the Federal Government to make a significant down-payment on adequately funding the nation’s alcohol and other drug treatment services in tonight’s budget.
“While there is some new funding for alcohol and other drug services – for example in Northern Queensland – without a national, strategic plan for the alcohol and other drug sector, how do we know that money is going where the need is greatest?
“Elsewhere the funding is about continuity of treatment services, but that’s not enough. We can’t just hold the line, we need to grow services to meet demand,” said Mr Hall.
19. $7M research funding to pilot new models of care for brain disorders in Australia
Statement by Mindgardens Neuroscience Network
The 2019 Federal Budget has delivered a win for people living with brain disorders in Australia, with a $7million funding boost for research aimed at developing improved models of care.
The clinical and research translation program, led by the Mindgardens Neuroscience Network (Mindgardens), will build new models of care to address the staggering burden of brain disorders in Australia. The disease burden associated with neurological, mental health and substance use disorders is in excess of $74 billion per annum and currently accounts for 20.5% of disability-adjusted life years, nearly twice the global figure of 11.1% illustrating the scale of the health care challenge. Between 2010 and 2017 substance misuse (drugs, alcohol) grew at 24.7%, followed by neurological disorders at 15.6% and mental health disorders by 8.6%.
Funding for Mindgardens will support a series of pilot programs to develop new models of care to target the three principal areas of brain health: (1) Neurological conditions, including developmental disorders, stroke and dementia, (2) Mental Health and (3) Drug, alcohol and addiction disorders.
Pilot programs will include Apex Clinics, a ‘one-stop hub’ assessment and review of all patients with neurological, mental health or addiction brain disorders; integrated community hubs, providing customised and targeted community services offering the best evidence-based care to patients and linked to general practice; innovative data technologies to build prevention tools to support early intervention for both the patient and the clinician.
Says Professor Helen Christensen AO, Interim Co-CEO of Mindgardens: “our current models of care treat individual disorders in a siloed manner. These disorders are frequently coexisting, they share brain mechanisms and behavioural patterns. We need to take a helicopter view that cuts across siloed service provision, creating better and more comprehensive care”.
Mindgardens, based in Sydney, Australia aims to become the Australian Comprehensive Brain Disorder Centre for clinical care, research and innovation where pilot programs like Apex Clinics, Integrated Community Hubs and Preventative Technologies can be developed and then rolled out nationally to support all Australians living with a brain disorder.
Professor Peter Schofield AO, Interim Co-CEO of Mindgardens says: “linking outstanding patient care with world-class research is the way to mutually leverage research discovery and treatment innovation. This has been demonstrated in cancer care where Comprehensive Cancer Centres have had great success in steering research towards the clinical problems of patients and bringing the benefits of research into patient care”.
“Our aim is to become an international leading precinct for innovative research and compassionate healthcare for all brain disorders,” says Professor Schofield.
20. New BBV/STI and AOD measures feature in Health Budget
Statement by the Australian Injecting and Illicit Drug Users League
AIVL has welcomed additional investments in blood borne virus (BBV), sexually transmissible infection (STI) and alcohol and other drugs (AOD) initiatives flagged in tonight’s Federal Budget. Funding for implementation of the new National BBV and STI Strategies and investment in a new Whole-of-Government Drug Strategy package have been announced as part of the Health Budget.
“The Australian Government has announced an additional $45.4 million over four years, commencing in 2019-20, to step up public health prevention and promotion activities around BBVs and STIs to deliver on the goals of the new National BBV and STI Strategies. The beneficiaries of this investment will be groups identified in the National BBV and STI Strategies, many of whom are particularly vulnerable members of the community,” said Melanie Walker, Chief Executive Officer (CEO) of AIVL.
“There is also $189.1 million in additional funding over five years, commencing in 2018-19, for a new Whole-of-Government Drug Strategy package to build on existing services and support, including in rural, regional and remote areas. This initiative includes funding recently announced for a national take-home naloxone program,” said Ms Walker.
According to the Health Budget papers, the new Drug Strategy initiative includes the following components that are additional to current funding in these areas:
- Rehabilitation services ($10.5 million);
- Increasing access to services in rural, regional and remote areas ($9.6 million);
- Providing local family drug support ($4.3 million);
- Reducing prescription opioid use through better access to pain management services ($4.3 million):
- PBS subsidised take home naloxone ($7.2 million); and
- National Ice Action Strategy ($153.3 million).
“In summary, the Health Budget looks good on first glance. AIVL looks forward to seeing more detail on planned spending and initiatives and engaging with the Australian Government and the Department of Health to ensure that implementation of the newly announced measures meets the needs of affected communities,” said Ms Walker.
AIVL is the national organisation representing people who use/have used illicit drugs and is the peak body for the state and territory peer-based drug user organisations.
21. Reaction from pharmacy groups
SHPA welcomes positive steps in medicine investment and aged care: statement
The Society of Hospital Pharmacists of Australia (SHPA) has welcomed focus on embedded pharmacy positions in aged care, investment in equal access to new medicines and improvements to hospital infrastructure and services after the release of the 2019-20 Federal Budget tonight.
SHPA Chief Executive Kristin Michaels says the adding of new cancer medicines to the Pharmaceutical Benefits Scheme and investment in clinical pharmacists in aged care are welcome aspects of the Budget, which was delivered by Federal Treasurer Josh Frydenberg in Canberra.
‘As outlined in SHPA’s 2018-19 Federal Budget submission, preliminary Australian evidence indicates a return on investment of $1.54 for every $1 spent embedding clinical pharmacists in aged care and we welcome the Federal Government’s allocation of $7.7 million in funding to help ensure greater access to their expertise regarding the use of medication, in particular inappropriate use of psychotropics and antibiotics.
‘As part of the $331 million over five years from 2018-19 for new and amended listings on the PBS, our members and their broader healthcare teams will enthusiastically welcome the addition of medicines to treat breast, blood and skin cancers and SHPA welcomes additional investment into the PBS-adjacent Life Saving Drugs Program, which is wholly managed by hospital pharmacists.’
‘Hospital pharmacists now facilitate more than 20 per cent of PBS expenditure and play a crucial role managing the introduction of cutting-edge medicines and the overall sustainability of this essential mechanism that improves equity of medicines access for all Australians.
Ms Michaels says it is surprising, given the increasing importance of medicines to the health of Australians, to see signs of proposed changes to hospital pharmacy pricing arrangements.
‘We are concerned at the short timeline of 1 July 2019 for potential implementation of any new pricing approach.
‘The proven efficiency and efficacy of hospital pharmacy stewardship of Australia’s growing medicines budget reaffirms the need for transparent negotiations and broad consultation with the whole pharmacy profession, given the potential impact of any such changes.’
There are 250,000 medicine-related hospital admissions each year in Australia, at a cost of $1.4 billion to the health system.
Ms Michaels welcomed the announcement of $107.8 million over seven years from 2018-19 to be invested into health infrastructure and services and $70.8 million for additional infrastructure and services to support the diagnosis, treatment and therapy for cancer patients.
‘The medicines management expertise of hospital pharmacists is pivotal in the effort to keep people out of hospital and SHPA also welcomes $1.3 billion over seven years for the Community Health and Hospitals Program, aiming to support patient care while reducing pressure on community and hospital services.’
***
Budget’s health funding welcome but more is needed for pharmacy: Statement by PSA
The government’s commitment to pharmacy in tonight’s 2019-20 Federal Budget through the extension of the AHI fee and reduced Pharmaceutical Benefits Scheme (PBS) wait times is welcomed by the Pharmaceutical Society of Australia (PSA).
PSA National President Dr Chris Freeman said PSA acknowledged the investment in primary care, aged care and mental health, and the importance of funding for those sectors.
“Leading into the next Community Pharmacy Agreement, we would expect at least the same level of investment in community pharmacy and pharmacists to improve accessibility of care and health outcomes for all Australians,” Dr Freeman said.
“In a budget that has now returned to surplus and is projected to be in surplus we need to have investment in pharmacy and pharmacists across sectors to improve the health of Australians.
“We note the budget announcement to align community pharmacy and private or public hospital pricing arrangements for high cost medicines but we remain concerned about the level of hospital pharmacy services that may be affected by this announcement and the impact this may have on medicine safety and patient care.
“PSA welcomes the government’s announcement of an additional $15 million for pharmacy programs through the sixth Community Pharmacy Agreement to promote quality use of medicines, including further supporting the Dose Administration Aids and MedsCheck programs.
“We are delighted the government will build on its efforts to reduce prescription opioid use. We welcome the expansion of the Rural Health Outreach Fund to give people better access to pain management specialist services and train providers to improve prescribing habits.
“The announcement of $7.2 million to establish an Australia-first take-home naloxone program is a significant investment in reducing deaths caused by opioids. It is vital for pharmacy to be a key component of this strategy.”
Dr Freeman said the establishment of a new unit of clinical pharmacists within the Aged Care Quality and Safety Commission that will work directly with residential aged care providers to educate them around best practice use of medicines will improve medicine safety across the country.
“We also welcome the government’s announcement of support for a Canberra trial to embed a part-time pharmacist in all 27 residential care facilities,” Dr Freeman said.
“Pharmacists have unique skills in medicines management and are the best placed professionals to ensure better use of medicines, focusing on regulation, education and intervention.
“The Budget begins to address PSA’s call in its pre-budget submission for $17 million of seed funding to embed pharmacists in aged care facilities.
“PSA has shown in our Medicine Safety report that medicine safety is a major problem in aged care, where 98% of residents are taking a potentially inappropriate medicine.
“Pharmacists embedded in aged care facilities can protect residents from the harm caused by overuse and misuse of medicines.
“We need a national commitment to ensure pharmacists are used to their full potential to lead a culture of medicine safety in aged care.
“The government’s announcement of funding for the continued operation of the My Health Record system is also a welcome investment that will allow people to access and control their medical history and treatments, including vaccinations.
“Nine out of 10 Australians already have a My Health Record and pharmacists are playing an important role in ensuring My Health Record delivers the efficiencies and effectiveness in healthcare that it has promised.”
22. MTAA welcomes Government’s commitment to health funding: statement
Medical Technology Association of Australia (MTAA), the peak industry body for medical technology has congratulated the Government and Health Minister for the commitments in the Budget handed down tonight.
MTAA welcomes the announcement tonight that $45.5 million will be spent on radiation therapy for regional Australia, something the medical technology industry has campaigned hard for.
Additionally, MTAA welcomes ongoing funding for Australia’s health and medical research sector, with $5 billion invested in the Medical Research Future Fund (MRFF) over 10 years to complement $3.5 billion for the National Health and Medical Research Council and $0.5 billion for the Biotechnology Translation Fund.
MTAA aims to ensure the benefits of modern, innovative and reliable medical technology are delivered effectively to provide better health outcomes to the Australian community.
The medical devices industry is committed to making a positive difference to the lives of the millions of Australians who benefit from medical technology every day.
MTAA welcomes the Government’s Budget commitment to:
$6 billion increase in funding for Medicare over the forward estimates
Increase in hospital funding over the forward estimates by $5 billion
Funding continued for information campaign on private health insurance reforms
$1.25 billion for Community Health and Hospitals Program to tackle service gaps including hospital infrastructure.
$1.1 billion for primary care including $449 million funding for general practitioners to provide flexible care (including telehealth) to patients over 70
Further funding for diagnostic Imaging including:
Increase to the Medicare rebate for diagnostic radiology and ultrasounds ($199 million) from 1 Jul 2020
23 new MRI licences
$32.6 million for breast cancer MRI and PET scans
$7.2 million to make fees for specialists more transparent
Funding for Cardiac, Breast Device and Hip Fracture registries
Funding for two new products for the Stoma Appliance Scheme
Expanding eligibility of the Continuous Glucose Monitoring program to new population with congenital condition under 21 years of age
$70.8 million to support Australians fighting cancer including the $45.5 million for new regional cancer treatment centres to provide radiation therapy
Continued funding of the National Health Funding Body to implement the National Health Reform Agreement
$7 million for the Mind Gardens Alliance to establish a brain disorders clinic in Sydney
A new Health and Medical Research Office to oversee the MRFF
$10 million for funding of research into Aboriginal and Torres Strait Islander Health
Ian Burgess, Chief Executive Officer of the Medical Technology Association of Australia said:
“MTAA congratulates the Government and the Minister for Health in the budget handed down tonight.
“The announcement that $45.5 million will be spent on radiation therapy for regional Australia is especially welcome and is something the sector has been calling for.
“We also welcome the Government’s ongoing commitment to Australia’s health and medical research sector through the Medical Research Future Fund.
“The medical technology industry welcomes the Government’s commitment to healthcare in Australia and we look forward to continuing to contribute to helping people live longer, healthier and more productive lives.”

23. Response from the Australian Nursing and Midwifery Federation
The country’s largest union, the Australian Nursing and Midwifery Federation (ANMF), described last night’s self-professed ‘back in black’ Budget, as a missed opportunity by the Morrision Government to provide safe, quality care for older Australians and fails to support the work of the nurses and carers who could make an actual difference.
ANMF Federal Secretary Annie Butler said the $21.6 billion for the aged care sector provides a patchwork of fragmented solutions but does not address the core issues underlying the widespread and systemic failures that have occurred across the sector and which are now being brought to light through the Royal Commission.
“The Government has made promises to support older Australians, invest in health and ensure essential services with this Budget, but has chosen to focus on tax cuts and a forecast surplus, which may or may not be delivered, instead of implementing measures which will actually turn those promises into reality,” Ms Butler said.
“The Budget has failed to direct health funding to those areas where it is urgently needed to alleviate the critical pressures being felt across the acute health system. And crucially, there is no genuine support to assist the nursing and midwifery workforce working in this system.
“Most critically of all there is no funding, no plan and no guarantee that this Budget will lead to improvements in quality and safety in aged care and there is definitely no support for the aged care workforce which is currently, under enormous pressure, just managing to hold the system together.
“The Government has once again failed to introduce legislative changes to ensure mandatory minimum staffing levels and hours of care for all residents, or to fund wage increases for nurses and carers to help build a quality workforce.
“This Budget is yet another missed opportunity for the Government to address the crisis in aged care by delivering crucial funding for additional staffing and guaranteeing that the generous taxpayer funded subsidies paid to providers are tied to direct care for residents.
“We believe that large, for-profit providers who continue to pay little or no tax, whilst taking advantage of their taxpayer-funded subsidies, should also come to the attention of the Government’s renewed crackdown on tax avoidance as announced in the Budget.
“There is little for nurses, midwives and carers to celebrate in this Budget, we only hope that the federal election will provide an opportunity for all sides of politics to genuinely recognise the value of their contribution to our society.”
24. Response from Aboriginal and Torres Strait Islander groups
(See a more complete wrap of responses here).
The National Aboriginal Community Controlled Health Organisation (NACCHO) said that funding for Aboriginal and Torres Strait Islander health was absent from Federal Budget.
NACCHO stated that it was disappointed at the lack of funding allocated in the 2019-2020 federal budget for Aboriginal and Torres Strait Islander health services and the Aboriginal Community Controlled Health Sector.
NACCHO welcomes the $15 million allocated for Indigenous suicide prevention and the $20 million for Indigenous specific initiatives for the implementation of the national strategies for blood borne viruses and sexually transmissible infections. However, we know that this commitment is well below the need.
“The gap between the health outcomes in Aboriginal and Torres Strait Islander peoples and other Australians will continue to persist unless there is a significant commitment to supporting the work of Aboriginal community controlled health organisations,” NACCHO CEO, Pat Turner said.
NACCHO has long called for an increase to the baseline funding for Aboriginal Community Controlled Health Services to support the sustainable delivery of high quality, comprehensive primary health care services to Aboriginal and Torres Strait Islander people and communities.
“We know that closing the gap will never be achieved until primary health care services are properly funded and our clinics have good infrastructure and are fit for purpose; until our people are living in safe and secure housing; until there are culturally safe and trusted early intervention services available for our children and their families; and until our psychological, social, emotional and spiritual needs are acknowledged and supported,” Ms Turner said.
“The physical and mental health and wellbeing of Aboriginal and Torres Strait Islander communities needs to be a priority for the Australian government. Our communities suffer disproportionately higher rates of suicide, cancer, kidney disease and obesity compared to non-Indigenous Australians,” Ms Turner said.
“We are disappointed that the Federal funding commitment does not match this critical need,” she said.
“We call on the all political parties to put Aboriginal and Torres Strait Islander health and full funding of the Aboriginal Community Controlled Health Sector at the heart of their election commitments.
Aboriginal Community Controlled Health Services provide at least three million episodes of care each year for about 350,000 people and employ about 6,000 staff.
“The life-saving and life-changing services our members provide have a tremendous impact on our communities. Without additional funding commitments from the Federal Government, our service capacity and reach are limited,” Ms Turner said.
******************************
The National Congress of Australia’s First Peoples released the following statement titled Australia’s First Peoples Need More Than Promises.
The National Congress of Australia’s First Peoples welcomes the Australian Government’s commitment of additional funding to address key challenges; however, the budget lacks concrete measures in areas of high importance for First Peoples. More needs to be done to remedy the structural causes of the gap between Aboriginal and Torres Strait Islander and non-Indigenous Australians.
National Congress is pleased with the commitment of $453.1 Million to the National Partnership Agreement on Universal Access to Early Childhood Education, and $276.5 Million to the Indigenous Youth Education Package as part of the Closing the Gap Refresh. However, we are concerned that the budget documents are vague in terms of implementation.
Simplistic measures such as school scholarships may be beneficial but are insufficient to overcome the structural challenges which Aboriginal and Torres Strait Islander children face at school including sharing our histories, languages and cultures.
While we welcome the commitment of $35 Million to fund Aboriginal and Torres Strait Islander-specific solutions to family violence, this must be provided to community-based and controlled organisations to be effective. Over 50% of our peoples have a disability and funding of $528 Million for the Royal Commission into disability services is welcome, provided our needs are taken into account.
Funding for the Lowitja Institute is welcome. While research is important, significantly more funding for services is required to address the disparities in health outcomes between Aboriginal and Torres Strait Islander and non-Indigenous communities. In addition, $5 Million over four years will be inadequate to remedy the incidence of youth suicide which afflict our communities.
National Congress is concerned by the amalgamation of funding for Legal Aid Commissions, Community Legal Centres and Aboriginal and Torres Strait Islander Legal Services under one National Funding Mechanism. In the past, amalgamation of funding for Aboriginal and Torres Strait Islander services under the Indigenous Advancement Strategy failed to deliver positive outcomes to our communities.
We are disappointed by the Australian Government’s continued rollout of cashless debit card trials. The $128.8 Million spent on the trials over the next four years would be better used to fund vital health, education and support services which enhance Aboriginal and Torres Strait Islander peoples’ self-determination instead of taking it away.
Dr Jackie Huggins, Co-Chair, National Congress said, “No progress has been made on the economic empowerment of Aboriginal and Torres Strait Islander peoples. The Government must ensure that Aboriginal and Torres Strait Islander peak organisations receive adequate funding to provide our peoples – the traditional owners of the land – with support, advice and representation.”
No increase to Newstart means recipients will continue to bear the enormous financial and emotional stress of not knowing if they will have enough for the bare necessities each week. Planned tax cuts have little impact on the disproportionate number of Aboriginal and Torres Strait Islander people who are low income earners.
There have been no changes to the Community Development Program; participants continue to work below minimum wage, and are in constant fear of being subject to harsh penalties for even minor breaches of program requirements. Money allocated under the Indigenous Advancement Strategy continues to be wasted on culturally inappropriate and ineffective services, while our organisations are forced to shut down due to lack of funding.
Mr. Gary Oliver, CEO, National Congress said, “The Minister for Indigenous Affairs’ budget press release boasts that the Indigenous Advancement Strategy has doubled the rate at which Aboriginal and Torres Strait Islander organisations deliver services. More than anything else, this highlights the Australian Government’s total failure to understand what Aboriginal and Torres Strait Islander peoples, organisations and communities require.
Our aim is not merely to increase the speed at which services are provided, but to ensure that they are effective; that they enhance our self-determination; and that our peoples and organisations are granted the opportunity to use our expertise to remedy the challenges which we uniquely face and understand.”
********************************
Centre of Best Practice in Aboriginal and Torres Strait Islander Suicide Prevention (CBPATSISP) Director Professor Pat Dudgeon and National Aboriginal and Torres Strait Islander Leadership in Mental Health (NATSILMH) Chair Mr Tom Brideson cautiously welcomed yesterday’s mental health and suicide prevention budget announcements but looked forward to more detail being released before committing to a response. Professor Dudgeon said:
I am especially pleased to see commitments to a National Suicide Information System. This is something that CBPATSISP and, prior to that, the Aboriginal and Torres Strait Islander Suicide Prevention Evaluation Project (ATSISPEP)called for. But it must operate in our communities and it’s not clear on the information provided whether it will. This is critical, such a system should help us get the people and resources to where they are needed faster, to help prevent suicide ‘clusters’, and better assist Indigenous families and communities after a suicide.
Professor Dudgeon also welcomed a $5 million commitment to an Indigenous leadership group to implement an Indigenous suicide prevention strategy; and similar funding for Indigenous youth leaders to respond to Indigenous youth suicide. She said:
A national Indigenous suicide prevention strategy was developed in 2013 and about $20 million implementation funding given to the Primary Health Networks (PHNs). While many PHNs are doing the best they can, the key ingredient – Indigenous governance and leadership in how that money is spent – has too often been lacking. It is my hope that the new Indigenous leadership group will not only lead a more effective and efficient national and regional response to Indigenous suicide, but also address these accountability problems. But again, we need more information about how these bodies will operate, and the leaders must be Indigenous and enjoy wide community support.
Mr Brideson called for greater funding for Indigenous mental health and suicide prevention:
$15 million Indigenous specific funding in a $461 million youth mental health and suicide prevention package, within a $736 mental health package, is not enough to meet our needs. Indigenous people comprise 3% of the population and have about double the suicide prevention needs, and three times the mental health needs, of other Australians. In terms of equity, we estimate about 9% of the total package, about $70 million, should be dedicated Indigenous expenditure. While this may seem a significant amount, it should not be forgotten that the bulk of Indigenous mental ill-health is preventable with access to primary mental health care, and yet the social costs of untreated Indigenous mental health difficulties are likely to run into the billions.
In fact, a long called for reinvestment funding approach to our mental health, particularly justice reinvestment, should eventually enable the Australian Government to make savings in many areas as well as making a big contribution to ‘Closing the Gap’ and Indigenous wellbeing. This is particularly in relation to the enormous cost of imprisoning over 13,000 Indigenous people, many of whom are in prison because of untreated mental health and related issues.
Professor Dudgeon and Mr Brideson closed by calling on Ministers Wyatt, Hunt and Scullion, their shadow ministry counterparts and the newly announced Suicide Prevention Coordinator to meet with them and other Indigenous mental health and suicide prevention leaders to discuss the detail of the package, and ensure that Indigenous peoples get their fair share of the mainstream elements of the mental health, suicide prevention, drug strategy and other budget initiatives:
We will be working with other Indigenous mental health and suicide prevention leaders to ensure our people, and young people in particular, benefit from all the budget measures according to their greater need. This includes the extra funding for headspace, the adult mental health centres and many other promising mainstream initiatives. CBPATSISP and NATSILMH want to see a partnership approach with the Australian Government to help ensure we get the detail right, and that the total $736 million package results in better mental health and suicide prevention outcomes for Indigenous Australians.
25. Palliative care
Palliative Care Australia (PCA) CEO Rohan Greenland says the time is rapidly approaching when all governments will need to substantially invest in palliative care as Australia’s ageing population increases and people continue to live longer with multiple chronic conditions.
“With the release of the updated National Palliative Care Strategy in February this year, all Australian governments made a commitment to ensure that evidence-based, quality palliative care is available to everyone who requires it.
“While the Budget delivered last night falls short on new funding for palliative care, PCA looks forward to working with whoever forms the next government to make sure there is funding to improve access to palliative care.
“Without a significant investment of funding and new models of care, under-served populations such as rural and remote Australians, Aboriginal and Torres Strait Islander People, culturally and linguistically diverse groups and people living with dementia or a disability will continue to miss out on the benefits of palliative care.
“PCA’s vision to enable access to quality palliative care for all Australians who require it by 2030, is a good foundation for systematic, workforce and funding reforms and we encourage those involved in implementing a number of the Budget measures to consider how they could help us achieve this vision.
“PCA is pleased to see a number of the Budget announcements that will improve quality of life and treatment options for people living with a life-limiting illness.
“This Budget also provides for a range of programs funded in the aged care sector that should include mechanisms to increase the provision of quality palliative care to the 60,000 Australians who die in aged care services each year.
“Particularly important is the aged care workforce strategy to ensure that aged care services have the right skill mix to be able to meet the palliative care needs of consumers, to reduce unnecessary transfers to hospital, and support staff to provide care to individuals and their families at the end of their lives.
“We also look forward to seeing the results of the funded trial to embed a pharmacist in residential aged care facilities. This is an important opportunity to consider the quality use of, and access to medicines required for adequate pain and symptom management if and when required at the end of life, which is an ongoing concern for PCA.
“The investment in medical research into ageing and unmet needs is also welcome. This should include a focus on palliative care research, which is needed now to prepare for our ageing population and to ensure that we are providing the best possible care to all people living with a life limiting condition.
“The clear focus in this Budget on investing in processes that support quality and safety for those accessing aged care services is important, however palliative care remains absent from the new Aged Care Quality Standards which we’d like to see included,” said Mr Greenland.








