Introduction by Croakey: “Ultimately, community health services have typically taken responsibility for the health and wellbeing of the whole community they serve in a way that other health services don’t, where the model is generally waiting for clients to come through the door.”
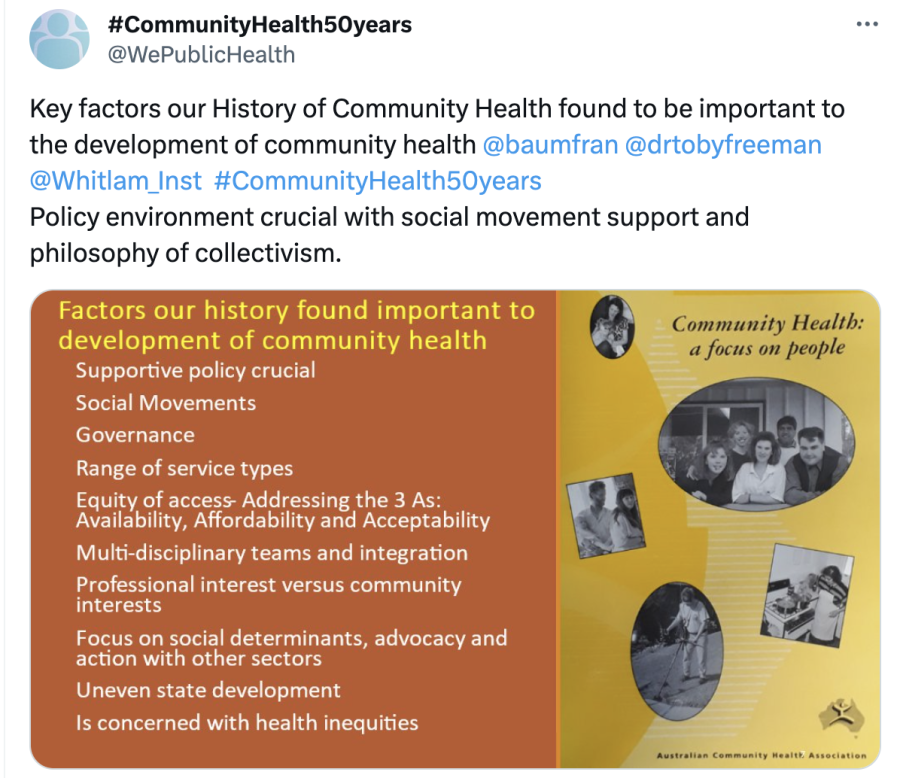
That’s one of many key takeaways from on community health from Professor Fran Baum, Dr Toby Freeman, and Dr Connie Musolino from Adelaide University’s Stretton Health Equity Institute, who took the helm at @WePublicHealth last week to mark the 50th anniversary of the Whitlam Government’s Community Health Program.
It culminated in a forum, held at the Whitlam Institute, that will inform an upcoming policy brief: ‘Lessons drawn from a history of community health services to inform current Australian primary health care policy’. Watch this space!
Fran Baum, Toby Freeman and Connie Musolino tweet:
We are very pleased to be tweeting about community health in the week we are going to celebrate the 50th Anniversary of the groundbreaking Whitlam Community Health Program emphasising prevention, community participation, multidisciplinary teamwork, social determinants of health.
What are community health services in Australia?
They focus on clinical services but also prevention, groups, community development, health promotion. They often have community members on their boards. They were first funded in Australia by the 1973 community health program under Whitlam.
Community health comes from a social view of health that acknowledges that the conditions in which people work, live, and play affect their health, and are shaped in turn by broader social structures and factors like poverty, racism, and urban planning.

Group work and community development
Two tools community health has used over the 50 years to tackle midstream and upstream factors affecting health are group work and community development. In line with the Ottawa Charter, they aim to build people’s skills and knowledge, and create supportive environments for health.
There are further examples in @DavidGLegge and others’ great 1996 book ‘Best Practice in Primary Health Care’, available for free at https://cdinhealth.org/resources/BPinPHC_B.pdf
Some examples of community health groups run over the decades include: domestic violence support groups, cooking groups, exercise groups, information groups, supermarket tours, early childhood playgroups and therapeutic groups, parenting groups and singing groups.
We have published a paper on the importance of group work in community health, which can take many different, complementary forms. https://onlinelibrary.wiley.com/doi/full/10.1002/hpja.323
Examples of community development in community health include community gardens, local action groups, tool libraries, arts and crafts, and IT classes.
We argue this means community development is critical for equity and safety, as it promotes access to needed services.
Community development has taken many forms in community health over the 50 years as well. It focuses on building skills, knowledge, and capacity in community so they have more control over their health.
There is much that group work and community development can achieve that individual 1:1 services can’t. Unfortunately, health system drivers mean they are undervalued, and harder and harder to get funded and supported.
Lastly, community development has been a strength of ACCHOs and other Aboriginal health services. Examples include lunch programs, arts, connection to Country trips, community forums on health issues, community collaborations e.g. on housing, racism.
Aboriginal community control
In Australia, the most vibrant, innovative, and long lasting model of community health has been Aboriginal Community Controlled Health Organisations (ACCHOs), which emerged out of Aboriginal social movements for self-determination and in response to a racist health system.

ACCHOs provide culturally safe health and medical care, disease prevention, and health promotion, as well as community development, advocacy, and action on social determinants, improving the health of Aboriginal peoples and communities.
The first ACCHOs pre-date the Alma Ata Declaration (1978) and the national Community Health Program (1973). Redfern AMS was established in 1971. @CAACongress (1973) and Pika Wiya and others followed soon after. Congress is now celebrating 50 years as well, and have amassed strong evidence of their contribution and the contribution of ACCHOs to Aboriginal and Torres Strait Islander Health.
Pika Wika, Congress, and Redfern are great examples of how the services were started by movements of local Aboriginal people, and struggled initially to gain funding from Australian governments e.g. https://pikawiyahealth.org.au/about-pika-wiya/…. The strengths of the model came years before funding.
If anyone manages to talk about community health or primary healthcare without mentioning ACCHOs, then they really haven’t been paying attention.
Focus on equity
Australia had a strong women’s community health movement from the 1970s onwards. A great history on this is Dorothy Broom’s 1991 book ‘Damned if We Do’ https://catalogue.nla.gov.au/catalog/1471868 that has a particularly good case study of the Leichhardt Community Women’s Health Centre.
Also great on this history is Gwendolyn Gray Jamieson’s book ‘Reaching for Health’ https://press.anu.edu.au/publications/reaching-health
Community health services in Australia were often consciously established in areas of socioeconomic disadvantage, to work with communities who struggled to access other primary health care, such as general practice.
Consider this example from one of our interviewees:

Equity was ingrained in community health’s ways of working from the start, and the goals community health was trying to achieve.
You may have come across frameworks like the 3As, or this more comprehensive one from Levesque et al https://link.springer.com/article/10.1186/1475-9276-12-18… that can be useful in reflecting on barriers and strategies to ensure equity.

We have also published this framework for evaluating what regional primary healthcare organisations can pursue to improve health equity in the population they serve https://link.springer.com/article/10.1007/s00038-018-1083-9

Critical to equity is community participation, health promotion, community development, and action on the social determinants of health. The problems need to be identified in the structures and environment, not the deficits of individuals.
It’s not just good for the health of the community to focus upstream, but it’s also been shown to be good for health professionals’ stress and burnout. See, for example, this article.
Some examples of strategies to improve equity of access over the decades include provision of creche, transport services, outreach, staff going to community events, free or very low cost services, ensuring services are on public transport routes, welcoming spaces and signage.
On welcome spaces, a great resource is Megan Warin’s SACHRU report ‘Not Just a Doctor’ https://catalogue.nla.gov.au/catalog/530762
Ultimately, community health services have typically taken responsibility for the health and wellbeing of the whole community they serve in a way that other health services don’t, where the model is generally waiting for clients to come through the door.
Community health has done lots of social action & advocacy to improve the health of local communities and involve them in management of health services. In 1998-90 Dale Street women’s health centre focused on home workers who were exploited.
One of the reasons community health is successful at improving the health of whole communities is community management.
Another defining feature of community health is multidisciplinary teams which ensure they have the skills to provide clinical, rehab, preventive and promotive health.
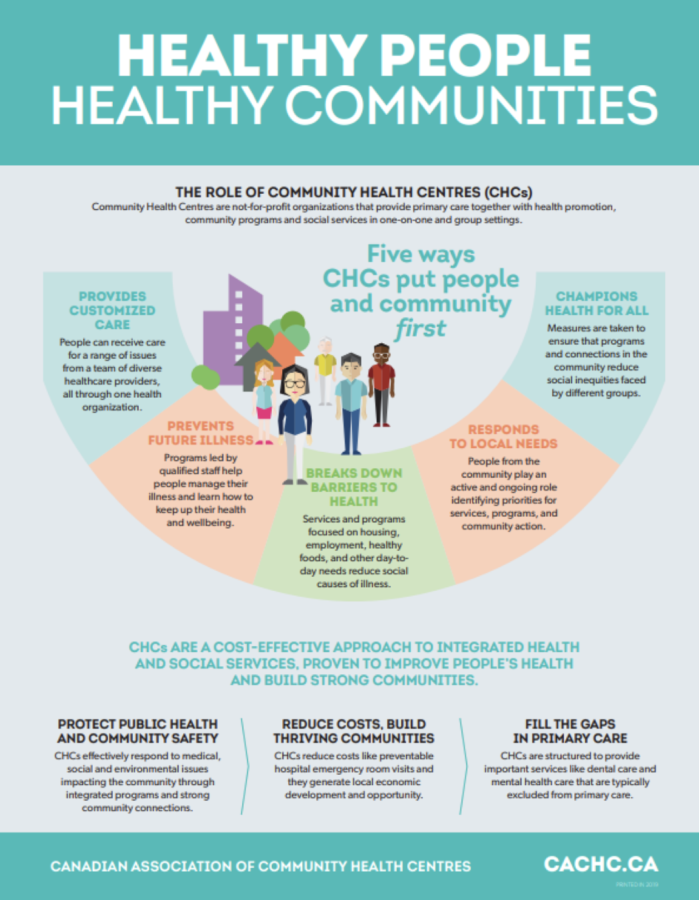
Community health is also thriving in #Canada. Their first centre was formed in 1926 and is now a network which recognises “that many differences in health status among segments of the population are socially and institutionally structured”. @CACHC_ACCSC
This is how the Canadian Community Health Centre Associations explains what community health is. Centres in Australia have had similar aims since Whitlam’s Community Health Program.
Good to see that community health is alive and well in Victoria. Community Health First is an initiative being led by all 24 registered independent community health services in Victoria to start a dialogue with Government.
Celebrating 50 years
 Today we are launching our interim policy brief ‘Lessons drawn from a history of community health services to inform current Australian primary health care policy’, to be updated after the forum. More to come… !
Today we are launching our interim policy brief ‘Lessons drawn from a history of community health services to inform current Australian primary health care policy’, to be updated after the forum. More to come… !
Quick tour of the @Whitlam_Inst Gough Whitlam exhibition before forum. Encourage everyone to visit. 50 years since landmark policies – free education, single mothers pension, family planning, introduction of the first health insurance – Medibank and of.course the community health program!
Prof John Juriansz Director of the @Whitlam_Inst opening the forum. 51 years since Whitlam Government swept into government with the catch phrase “It’s Time”. The It’s Time speech highlighted how unequal the former Liberal health policy was.
In response the Whitlam Government brought in a suite of innovative health policy and programs – perhaps the most radical was the federal Community Health program in its new models of service delivery.
Community control and accountability in every aspect of governance crucial to success of community health centres and services.
@baumfran outlines the shift from a comprehensive primary healthcare model to a selective health model, both in the mainstream health system & community health.

The Hon Mark Butler reflects on Gough Whitlam modernisation of the Labor Party in the 70s, as a vehicle to modernise policy reform agenda and Australian society.

He says many of the same issues identified in the 1973 Health Commission calling for community health were similarly identified in the recent 2033 Strengthening Medicare Taskforce report.
Conversation about #communityhealth50years between @baumfran and @Mark_Butler_MP – wonderful to have a health minister who understands the values of community health services.
Strengthening Medicare will fund new rebate and bulk billing to address inequities in access, increase funds to consumer bodies: CALD and mental health consumer bodies, invest in multidisciplinary teams, invest in Urgent Care clinics to address “local needs”.
Whitlam would have been mightily pleased with how Aboriginal Community Controlled Health Services have developed, as Tamara MacKean explains.

The growth of women’s health Centres described by @ConMusolino – feminist movement was vital in shaping them. A big advantage of women’s health Centre is that they work at the intersection of oppressions.

The sad decline of community health in #SouthAustralia described by @drtobyfreeman. Whitlam would not be impressed!

There has never been a more supportive political environment for community health than under the Whitlam Government.
Dr Ben Harris-Roxas on co-commissioning challenges = lack of shared understanding of what community health is, lack of visibility of community health and counting it. Challenge of doing it in a way that doesn’t cause fragmentation. Whitlam CH program enabled continuity of care.
Tony McBride – community health centres were essential in COVID response. Victorian community health services continue to work with the community in governance and this feeds into services and ability to respond to local needs.
A/Prof Tamara Mackean on importance of social movements to Aboriginal community controlled health. Highlights importance sovereignty, place and connection to ACCHOs’ strength.
Kent Burgess CEO of Your Community Health talking about difficulty of fragmented and unstable funding including that it can undermine relations with community they serve and undermine trust.
Questions from the room – what movement do we need to get community controlled health model for all Australians?
@baumfran Plant seeds in the community, look to current consumer health movement at the moment growing, need to look for universal schemes, continuing funding streams.
A/Prof Tamara Mackean discussing social concepts of wellbeing. Aboriginal Waljen central desert people have collective understandings of health, experience health as collective, and recognise we are all interconnected.
Dr Ben Harris-Roxas – Community development model central to the community health program will be central going forward as we deal with social, health and climate crisis coming ahead.
Gough said it 50 years ago and it is still true today: “Health is a Community Affair”.
This is the team which produced the research behind the #communityhealth50years celebration: @drtobyfreeman @ConMusolino @baumfran @DavidGLegge Tony McBride, Paul Laris, Denise Fry, Tamara MacKean, Jenny MacMillan, Warwick Anderson, Jamie Dunk – Virgina Lewis was overseas.




Stretton Health Equity team signing off. Thanks to everyone who followed #communityhealth50years. We were glad to partner with the @Whitlam_Inst to be part of their celebration of the 50th Anniversary of Gough Whitlam’s reforming government that changed Australia for the better.
See Croakey’s archive of articles on community health








