Introduction by Croakey: Australia’s political leaders have been urged to come together in bipartisan efforts to stop the spread of COVID in a powerful article in the medical publication Insight, titled ‘Time to put people ahead of politics’.
Dr Jillann Farmer, a Brisbane-based GP and former Medical Director of the United Nations, documents the many ways that public health responses to the pandemic in Australia have been undermined, weakened and discarded.
“It’s time for our medical leaders to give strong and assertive advice to politicians, to leave them no plausible deniability, and for politicians to explain their reasoning for rejecting clear medical advice,” she writes. “We need our political leaders to come together in bipartisan efforts to stop the spread and avoid the temptation of wedge politics when lives and the future health of the nation are at stake.”
The article was published before revealing photos emerged from the 47th Parliament (published in Croakey’s #ICYMI column) showing a stark political divide in mask wearing.
Some of the political barriers to public health action are outlined by Frank Bongiorno, Professor of History at the Australian National University, in an eloquent article at The Conversation.
He writes:
These are difficult matters for governments that would much prefer to get on with something other than boring old pandemic management. The issue is entangled in electoral politics – we have just had a federal contest in which major party leaders studiously ignored the issue, and the nation’s two most populous states are to hold elections in the next few months. Governments also realise that restrictions and mandates will meet civil disobedience.
But COVID cannot be wished away. At a minimum, governments need to show they are serious about it to the extent of spending serious money on a campaign of public information and advice on issues like mask-wearing and staying home when ill.”
Meanwhile, leading public health experts provide a timely brief below on the evidence to support indoor masks, together with vaccines, clean air and isolation, as a powerful tool to reduce COVID-19 transmission. They join growing calls for political leadership to act on the public health evidence.
Michael Toole, Margaret Hellard, Nancy Baxter, Raina MacIntyre and Brendan Crabb write:
It is clear that Australia is in the midst of another wave of COVID-19 fuelled by the now dominant BA.4 and BA.5 sub-variants of Omicron. Death rates are extraordinarily high; an average of 68 per day and rising, and acute and chronic illness from COVID is so substantial that the healthcare system more generally is compromised. Indeed, no sector in our society remains untouched.
Cases are up sharply, now over 50,000 each day, and the increase in hospitalisations is crystal clear. Currently, more than 5,500 Australians are in hospital with COVID-19, surpassing the previous peak in late January. During the past seven days, Australia has had the second highest deaths per capita in the world, excluding small island states.
Given the urgency of the need to reduce transmission and reduce COVID cases, we simply must maximise use of the few key tools we have; vaccination, masks, ventilation, and testing (so you can isolate and, if eligible, get treatment if positive). We are currently falling short on all fronts. (See this graph of hospitalisations in The Guardian Australia).
During the first two years of the pandemic there were distinct waves as new variants such as Alpha and Delta emerged globally and inevitably in Australia. Omicron is a game-changer. There are no longer clear gaps between waves with daily case numbers never reaching below 22,000. The UK Office for National Statistics has estimated that reinfections by the Omicron variant have been seven times higher than during the Delta wave.
What can we do to reduce the impact of the current wave?
First and foremost, we need to increase coverage by third dose boosters and, among the eligible, fourth doses. The current third dose rate has stagnated at around 70 percent for some time; this ranks 35th in the world.
Only 63 percent of Australians over 65 have received a fourth dose compared to more than 95 percent with two doses. The fully vaccinated rate in children aged 5-11 years is even lower, hovering at 40 percent.
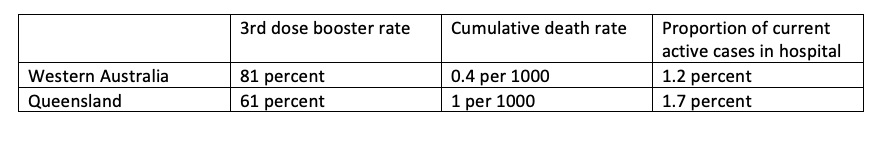
It’s interesting to look at the impact of boosters on severe COVID-19 outcomes in two Australian states that started their COVID experience with Omicron as shown in this table. Both outcome indicators are significantly higher in Queensland than in WA. Three and four dose vaccination remains a very powerful protective force against severe disease and death from Omicron infection.
Vaccines Plus
It is not only a longstanding principle in the control of epidemics that the response be multi-pronged, our experience with COVID-19 makes it clear that one intervention is not enough, either for the individual and certainly not for the community.
In the current escalating phase of the COVID-19 pandemic, the following measures should be employed and made available to all communities to reduce circulating virus and to prevent severe illness:
- Increase 3rd and 4th booster vaccination coverage in adults and second doses in children 5-11 and recommend vaccination for children 2 months to 4 years
- Maintain and strengthen testing, including ramping up PCR testing for symptomatic people whose rapid antigen tests (RATs) are negative and making RATs affordable and widely accessible
- Expedite and expand access to subsidised oral antiviral drugs
- Actively promote and provide indoor mask wearing, emphasising P2/N95 masks
- Improve indoor ventilation.
To empower people to understand the benefits of these measures, health promotion, both through mass advertising campaigns and community engagement, is essential. At the very least, political leaders need to be seen wearing masks in public appearances. Moreover, flexible working arrangements are important to reduce transmission risk in workplaces.
We do not include work at home orders in this list as we consider them a symptom of failure to implement the other measures. Nevertheless, individuals may consider that working from home offers them the best protection.
Methods to reduce the concentration of SARS-CoV-2 particles in indoor air include ventilation, filtration, and disinfection. In a 2020 study of Georgia (USA) elementary schools, COVID-19 incidence was 39% lower in 87 schools that improved ventilation compared with 37 schools that did not. Victoria is the only state that has significantly invested in better ventilation in schools.
In a recent study, the combination of well fitted respiratory masks (N95) and air filtration devices reduced Covid-19 transmission to near zero. However, this was in highly controlled health care settings.
Evidence for effectiveness of masks
A number of studies in 2020 and 2021 established the evidence base for masks. Published by the Royal Society in June 2020, a review of pre-pandemic studies found that all types of masks reduced transmission of respiratory viruses. The authors noted that ten randomised controlled trials (RCT) of masks all had sample sizes that were too low to demonstrate effectiveness and did not include them in their analysis.
In February 2021, a review found that wearing a mask provided up to 79 percent protection against infection by SARS-CoV-2, the virus that causes COVID-19. However, the studies did not differentiate between different types of mask. Like the previous review, this study excluded RCTs for the same reason.
In September 2021, a landmark clinical trial in 350,000 people in rural Bangladesh found that surgical masks — but not cloth masks — reduced transmission of SARS-CoV-2 in villages where the research team distributed face masks and promoted their use. This is one of the few published clinical trials with a sample size large enough to demonstrate statistically significant mask effectiveness.
A modelling study in the USA found that when masks are used in the community at rates of 80 percent for those older than 65 years and 60 percent for those under 65 years, face masks are associated with reductions in COVID‑19 infections of 69 percent for cloth and 78 percent for surgical masks.
An Australian study found that mandating masks during Victoria’s second wave in 2020 was the single-most important control measure (pre-vaccination). The researchers found that the introduction of mandatory mask use while Stage 3 restrictions were in place, turned an exponential increase in community transmission into an exponential decrease.
A 2022 study by the Burnet Institute found that a 20 percent reduction in transmission (via a package of test-isolate, indoor masks and increased vaccine booster rates) could save 2,000 lives across Australia. More recent modelling, not yet published, found that mask wearing by more than 50 percent of the population would make a significant contribution to that reduction.
However, it is important to point out the benefits of respiratory masks over cloth or ill-fitting surgical masks. A study in California showed that a N95 respirator provided 83% protection compared to 66 percent from a surgical mask and 56 percent from a cloth mask.
One of the most contentious issues in this phase of the pandemic is whether indoor masks should be mandated rather than merely recommended. A study of three countries including Australia showed a mandate greatly increased rates of mask wearing. There is also the effect of peer pressure, where some people who want to wear a mask are embarrassed to do so when no-one else is wearing one.
One of the most compelling reasons to mandate indoor masks comes from organisations representing exhausted healthcare workers. Many, such as the Rural Doctors Association, are urging mask mandates to help alleviate their unsustainable workloads. Hospitalisations are a predictable percentage of cases, so reducing case numbers by using the above measures will also ease the burden on the health system.
Calling all leaders
The current phase of the COVID-19 pandemic, with escalating infections, hospitalisations and deaths, demands a comprehensive public health response to reduce the impact on the healthcare system and society more broadly. This wave may not have yet peaked and there are likely to be more waves to come so we need to be well prepared.
We already saw cascading failures in the health system, supply chains, schools and many parts of society in January and February.
Failing to use all the tools available to reduce transmission in the community will negatively affect the economy as more and more people isolate and absenteeism surges. Now is the time for clear messaging and evidence-based and minimally disruptive mitigations.
Most critically, we need leadership from the Prime Minister and Premiers, Chief Ministers and Ministers of Health in all nine jurisdictions to motivate the public to undertake the desired behaviour change necessary to achieve a reduction in community transmission of the virus.
Authors
Professor Michael Toole is an Associate Principal Research Fellow at the Burnet Institute.
Professor Margaret Hellard is the Deputy Director for Programs at the Burnet Institute.
Professor Nancy Baxter is Head of the School of Population and Global Health, University of Melbourne.
Professor Raina MacIntyre is Head of the Biosecurity Program, Kirby Institute, University of New South Wales.
Professor Brendan Crabb is the Director and CEO of the Burnet Institute.
See Croakey’s extensive archives on COVID-19






